What to Know Before Getting a Vasectomy
Getting a vasectomy, sometimes called male sterilization, is a decision that more men are choosing to make, with an 850% increase for the search term "where…

Update your location to show providers, locations, and services closest to you.
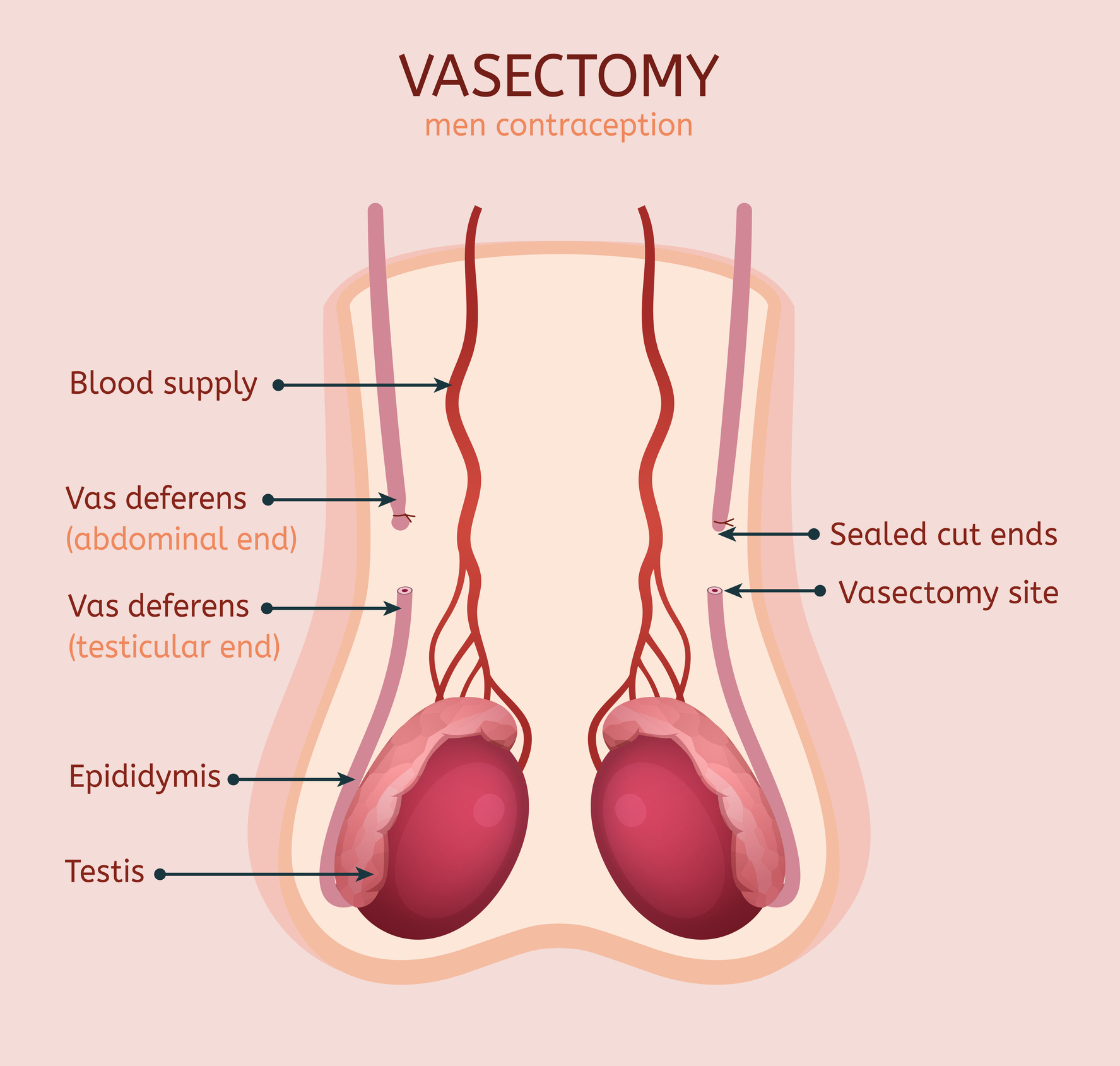
Each year, over 500,000 men in the United States undergo a vasectomy, and each year, 6% of those men undergo a vasectomy reversal. Reversals are done in an outpatient setting using a surgical microscope. A general anesthetic is required to assist with the fine dissection and anastomosis of the lumens of the previously occluded vas deferens. An incision is made on each side of the scrotum to reveal the site of the previous vasectomy. The occluded segment is removed, and the two fresh ends are joined using stitches as thin or thinner than a human hair.]
There are two types of reversal procedures:
You have chosen to have a vasectomy reversal. The information below will help you understand your surgery, what will happen in the hospital and what you can expect when you go home. You can also find your plan of care from your doctor.
The success of a vasectomy reversal depends on the skill of the surgeon and the findings at the time of surgery. A surgeon should be trained in microsurgical technique, as precise suture placement and intraoperative decision making a crucial to the success of the surgery. The surgeon must also have the ability to perform the more difficult epididymovasostomy procedure pending the findings at the time of surgery. The more time elapsed since the vasectomy, the more challenging the procedure may be as secondary obstruction in the epididymis can occur from prolonged increases in pressure from the blocked vas deferens.
The procedure is performed by opening the previously blocked ends of the vas deferens and sewing the fresh edges together to create a patent channel for sperm to pass through. The defect in the vas deferens created by the vasectomy can sometimes be palpated through the scrotal skin. An incision is made vertically (up and down) on each side of the scrotum to reveal the previous site of the vasectomy. This incision is generally 2 inches. If the amount of vas deferens removed at the time of surgery was extensive, the incision may need to be extended upwards towards the inguinal canal.
The blocked ends of the vas deferens are incised to allow fluid to flow from the testicular side of the vasectomy site. If sperm are present, then 90% or more of patients are expected to have return of sperm in the ejaculate with a 60% to 70% pregnancy rate. If no sperm are present, yet the vasectomy fluid is abundant and appropriate for sperm production (clear, watery), then a vasovasostomy is also performed with direct attachments of the two ends of the vas deferens. If poor-quality fluid is present (thick, pasty), and no sperm are found, then the abdominal side of the vas deferens is connected to the epididymis by performing an epididymovasostomy. The anastomosis (new connection that is created) is performed in two layers using microscopic sutures the size of a human hair. This is done using high definition surgical operating microscopes.
If you had previously discussed banking sperm or a testicular biopsy, this is also performed through the same incision. Cryopreservation is performed in this way as a safety backup in the event that inadequate sperm counts are present after surgery.
Additional information on vasectomy reversal (PDF).
You may need to have an evaluation before surgery at UF Health Shands Hospital on the 1st floor. The evaluation is made up of a physical exam, chest X-ray, blood tests, urine tests, an Electrocardiogram and other tests necessary for your health and safety before surgery. At the time, you will be able to ask questions about your medications and hospital care. You will be told about which medications you should take and which you should not take before surgery. Please bring your medications in their original bottles to the before surgery evaluation.
If you take medications that cause clotting of the blood such as Coumadin, Plavix, Aspirin, Vitamin E, fish oil, or any NSAID (i.e.: Motrin®, Aleve®, Advil®, ibuprofen), these medications should be reported to your doctor and the person giving you medications. For your safety, these types of medication should not be taken for a least a week before surgery.
The day before your surgery, you may eat a light breakfast (no later than 11 a.m.). After breakfast, begin drinking clear liquids (Sprite®, 7up®, ginger ale, apple juice, tea, Jell-O®, ice pops, Gatorade®, chicken or beef broth) for the rest of the day then nothing by mouth after midnight.
To find out what time you need to be at UF Health on the day of your surgery call (352) 265-0023 between the hours of 7 p.m. and 11 p.m. the day before surgery.
On the day of surgery, you will get to UF Health at the time you were told. The check-in area is on the first floor at the Ambulatory Surgery Check-In desk. You will be taken to the before surgery holding area next to the operating room.
Once you are taken into the operating room and the surgery starts, the family can call from the Surgery waiting area on the first floor and get updates from the operating room every one to two hours. Your family members must be prepared to wait.
The surgery itself takes about three hours to perform. However, it takes at least one to two hours to get you ready for the surgery, and you will spend anywhere from one to two hours after surgery in the recovery room.
After surgery, the doctor or a member of the surgery team will talk to your family either in person or by phone. At least one family member should stay in the Surgery Waiting Area on the first floor at all times for the entire surgery so that your doctor can locate them and give them an update on your condition once the surgery is over. If none of your family members are in the waiting area then your doctor will not know where to find them.
Call your doctor if you have:
During work hours (8 a.m. to 5 p.m. Monday through Friday), call the UF Health Urology Clinic at (352) 265-8240.
After hours or weekends: Call the UF Health Shands operator at (352) 265-0111 and ask for the urology resident on-call.

Getting a vasectomy, sometimes called male sterilization, is a decision that more men are choosing to make, with an 850% increase for the search term "where…
