TIF- Transoral Incisionless Fundoplication
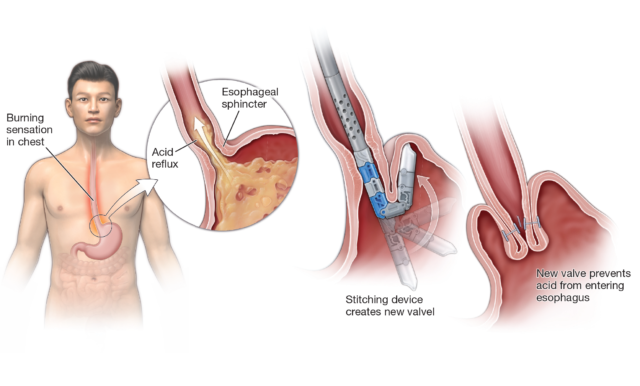
Transoral incisionless fundoplication (TIF) is an advanced endoscopy procedure that delivers relief from chronic acid reflux or symptoms of acid reflux, such as heartburn or regurgitation, associated with gastroesophageal reflux disease (GERD). The TIF procedure uses an endoscopic approach to reconstruct the gastroesophageal valve (GEV) without incisions.
The procedure
During the TIF procedure, the patient is placed under general anesthesia. A flexible, tube-like imaging instrument known as an endoscope is fed through a special TIF device that is preloaded with forceps and plastic fasteners. Together, the endoscope and TIF device are passed through the mouth, down the esophagus, and into the stomach, allowing the physician to repair or reconstruct the body’s natural barrier to reflux (the anti-reflux valve) at the gastroesophageal junction. The TIF device allows the physician to grab the end of the esophagus and pull it down so that the top of the stomach can be wrapped 270 degrees around the esophagus and secured with a plastic fastener that remains in the body. The procedure takes up to one hour.
Why consider TIF
GERD is a very common medical condition affecting up to 20% of the general population. The main symptoms of GERD include burning sensation behind the chest and/or regurgitation of stomach content into the throat and mouth.
Untreated, GERD can be very bothersome. It may predispose patients to damage in the esophagus and can increase the risk of developing esophageal cancer.
Most patients with GERD can be managed with medications and life-style changes. Proton pump inhibitors, PPIs, are most commonly used. These medications include omeprazole, pantoprazole, esomeprazole and others.
While these medications are highly effective, long term use of PPIs may rarely be associated with adverse events including:
- Inflammatory bowel disease
- Atrophic gastritis
- Microscopic colitis
- Malabsorption of magnesium, calcium, B12 and Iron
- Bone thinning and fracture
- COVID-19
- Dementia
- Pneumonia
Eligibility
You are eligible for TIF if you meet some of the following criteria:
- Age is > 18
- Daily, bothersome GERD symptoms (> 1 year) despite medical therapy (> 6 months)
- Anatomic disruption
- Proven GERD by either endoscopy or ambulatory pH study
- Hiatal hernia is less than 2cm in size
Benefits of TIF
TIF has many benefits, which include:
- It is minimally invasive with no surgical cuts
- Shorter recovery time
- Can treat GERD symptoms
- Can be off medications
Procedure Success
Multiple national studies indicated that the TIF procedure is performed successfully in up to 99% of patients, with just 2% experiencing issues during or after the procedure, such as a tear or internal bleeding.
For most patients, TIF provides significant GERD symptoms relief and improved quality of life.
Typically, symptom relief after TIF lasts from 9-10 years. When GERD symptoms return, some people may need to repeat TIF, resume taking proton pump inhibitors (PPIs) or explore other treatments.
Alternatives
Continued medical management-- Includes continuing PPIs or other medications
Life-style changes-- Include avoiding caffeine, elevating the head of the bed, avoiding citrus or acid drinks, and avoiding eating 3 hours before bed-time.
Surgical management-- There are various surgical options to manage GERD. All of them include some surgical cutting.
Before the Procedure
Do not eat or drink for 12 hours before the procedure to clear your esophagus of food products.
Inform doctor of any allergies.
Follow doctor instructions whether to continue taking prescription medications.
Day of the Procedure
- Take blood pressure, heart and GERD medications in the morning of your procedure with a sip of water
- Do not take Maalox, Mylanta, Carafate/Sucralfate or Metamucil the morning of the procedure
- Bring insurance card and current list of medications
- Place scopolamine patch behind either ear to prevent nausea
After the Procedure
Typically, the patient will go home the same day or the following day, depending upon the individual situation and the recommendations of the physician. Typically, the patient can return to work in 3-7 days, unless strenuous work.
- No strenuous activity or activity that increases abdominal pressure or core exercise during your healing (no lifting heavy items >5 pounds for two weeks, >25 pounds for three weeks)
- Avoid smoking
- Take antibiotics as prescribed by doctor
Diet: First 24 hours, eat and drink only clear liquids. First week-- liquids only; second week—soft foods; third week-- progress to a regular diet, with small-sized meals. Avoid all breads and meats.
Common symptoms post-procedure
These symptoms should improve every day:
- Stomach discomfort
- Nausea
- Sore throat
- Shoulder pain
- Minimal chest discomfort
- Minimal chance of bleeding
Procedure Cost
The procedure is covered by most insurances. Out-of-pocket costs vary based on the patient’s insurance.