The Year in Review: Celebrating Our Achievements in 2016 Part 2
Part 2 of our “Year in Review” focuses on the hospitals, research institutes and centers that are part of the UF Health family:
- UF Health Cancer Center
- UF Clinical and Translational Science Institute
- UF Institute for Child Health Policy
- The UF Diabetes Institute
- UF Emerging Pathogens Institute
- UF Genetics Institute
- UF Institute on Aging
- Evelyn F. & William L. McKnight Brain Institute
- UF Health Shands
- UF Health Jacksonville
UF Health Cancer Center
Director: Jonathan D. Licht, M.D.
 The University of Florida Health Cancer Center has undergone substantial change this past year under the leadership of Jonathan D. Licht, M.D., who began as director in October 2015. Noting the excellent potential of the university and the academic health center to achieve National Cancer Institute designation as a cancer center and using state-provided resources, he started a reorganization of the Cancer Center. In February 2016, an external advisory board consisting of leaders of NCI-designated cancer centers from across the country was convened to evaluate the major characteristics of a successful NCI center. These included: 1) the organization and leadership of the center, 2) basic and clinical research space, 3) development of collaborative cancer programs, 4) cancer focus — the size and scope of basic, clinical and population sciences based cancer research at UF, and 5) institutional commitment.
The University of Florida Health Cancer Center has undergone substantial change this past year under the leadership of Jonathan D. Licht, M.D., who began as director in October 2015. Noting the excellent potential of the university and the academic health center to achieve National Cancer Institute designation as a cancer center and using state-provided resources, he started a reorganization of the Cancer Center. In February 2016, an external advisory board consisting of leaders of NCI-designated cancer centers from across the country was convened to evaluate the major characteristics of a successful NCI center. These included: 1) the organization and leadership of the center, 2) basic and clinical research space, 3) development of collaborative cancer programs, 4) cancer focus — the size and scope of basic, clinical and population sciences based cancer research at UF, and 5) institutional commitment.
The External Advisory Board’s highly encouraging report was received in April 2016 and offered specific suggestions for shaping programs. After analysis by Dr. Licht and colleagues, the center was organized into four research programs:
a) Cancer Therapy and Immuno-oncology — Led by Duane Mitchell, M.D., Ph.D. b) Cancer Microbiome and Host Response — Led by Christian Jobin, Ph.D. c) Cancer Genetic and Epigenetic Integrity — Led by Robert Hromas, M.D. d) Cancer Population Sciences — Led by Betsy Shenkman, Ph.D.
Over the summer, faculty in the programs began regular meetings to encourage collaboration and coordination of research. At the same time, recruitment occurred at a brisk pace: eight new laboratories were started in the past year, representing collaborative recruitments between the Cancer Center and the departments of Biochemistry, Pharmacology, Cell Biology and Anatomy and Medicine (College of Medicine), Medical Chemistry (College of Pharmacy), Oral Biology (Dentistry) and Chemistry (Arts and Sciences). In addition, several new population sciences researchers were recruited in Epidemiology and Health Services (Public Health and Health Professions) and Journalism and Communications. Notable new awards include a Department of Defense Advanced Regenerative Manufacturing Institute, led by engineering professor Greg Sawyers, which has a cancer focus in cooperation with the department of orthopaedics and rehabilitation and external collaboration with Dean Kamen, the inventor of the Segway. NCI funding for the UFHCC now stands at $10 million and cancer-related funding at nearly $30 million. To accommodate new faculty recruits in the coming years, 8,000 square feet of new space was recently completed on the ground floor of the Basic Sciences Building.
The Clinical Trials office is undergoing reorganization in cooperation with the Clinical and Translational Science Institute, and clinical trials accrual is increasing, with nearly 10 percent of new patients enrolled on interventional therapeutic, diagnostic or supportive trials.
The UF Health Cancer Center Leadership has undergone change. Dr. John Wingard has been named deputy director of the Cancer Center, focusing on alignment of clinical research programs, center membership and strategic planning. Dr. Thomas George, of the Division of Medical Oncology, has been named associate director for clinical investigation, serving as the faculty supervisor of the clinical trials office and developing an early phase cancer trials unit. Dr. Elizabeth Shenkman serves as interim associate director for population sciences, leveraging her OneFlorida program, which studies how real-world clinical practice responds to new research advances. She is coordinating colleagues in Nursing, Epidemiology, Journalism, Health Services Research and other groups to address the important issues of cancer prevention, communication and palliation. A new director for administration, Bob Houlihan, will start in March 2017. Mr. Houlihan has nearly a decade of experience as the chief research administrator of the NCI-designated Massey Cancer Center of the Virginia Commonwealth University, where he recently played a major role in the renewal of its NCI grant. The Cancer Center clinical trials office will be led by Alison Ivey, R.N., who will work closely with former director Brian Sevier, Ph.D., who will now lead the campuswide clinical trials enterprise. Dr. Parker Gibbs has moved from the position of associate director for clinical affairs of the Cancer Center to become the Chief Medical Officer of UF Health Shands, and plans to recruit his successor are being made.
The Cancer Center’s education and mentoring program is continuing to develop with an ongoing minority training program under Dr. Folakemi Odedina, funded by a P20 grant and a soon-to-be-awarded R25 grant. The Cancer Biology curriculum for the interdisciplinary graduate program continues to develop under the leadership of Dr. Dietmar Siemann. This year at the annual UF Health Cancer Center Research Day, five highly competitive $10,000 dissertation prizes were awarded to Ph.D. students who had passed their qualifier exams to help fund their research. The students presented their projects in concise three-minute talks that were enormously well-received by the nearly 200 attendees of the retreat. In addition, travel awards were given to best poster among the students, postdoctoral fellows and junior faculty who presented their work.
The Cancer Center has continued to work with partners at the UF Health Proton Therapy Institute, installing additional clinical research staff at that center to facilitate the development of prospective clinical trials. A collaborative agreement was signed with Orlando Health to enable investigator-initiated clinical trials to be opened at that center under the UF umbrella. Lastly, as encouraged by the state of Florida Cancer Preeminence effort, the center has a number of robust collaborative projects with our colleagues at the University of Miami and Moffiitt Cancer Center.
In summary, the University of Florida Health Cancer Center is well on its way to achieving NCI designation with the programs, structures, grant portfolio and clinical trial enrollments all reaching the benchmarks needed to be competitive for this award. With several key recruitments to come and another one to two years of program development, we anticipate submission of an application to the National Cancer Institute.
Clinical and Translational Science Institute
Director: Dave Nelson, M.D.
 As a catalytic hub for translational research, the CTSI leads transformative programs, provides services and resources for research teams, and offers a broad range of training and education opportunities. Last year the CTSI served close to 1,000 investigators, and more than 200 scientific publications were published about research facilitated by CTSI resources.
As a catalytic hub for translational research, the CTSI leads transformative programs, provides services and resources for research teams, and offers a broad range of training and education opportunities. Last year the CTSI served close to 1,000 investigators, and more than 200 scientific publications were published about research facilitated by CTSI resources.
In 2016, the CTSI developed a three-year strategic plan to operationalize five goals in pursuit of its mission. Highlighted accomplishments toward advancing each goal are summarized below.
CTSI accomplishments reflect the dedication of hundreds of faculty, staff and students from across the university and at partners throughout the state, including Florida State University, the University of Miami and affiliated health care providers through the OneFlorida Clinical Research Consortium.
UF Translational Research Environment
Continuously improving the translational research environment at UF is central to the CTSI’s mission. Notable accomplishments under this goal in 2016 include:
Human Subject Research Taskforce: Informed by peer benchmarking and stakeholder input, the CTSI partnered with key units and institutional leadership to develop a three-year plan for implementing two of the task force’s recommendations for improving human subject research processes: implementing OnCore as an enterprise-level clinical research management system and reorganizing UF’s clinical research resources and administration under a new Office of Clinical Research.
Research Services and Resources: CTSI Service Center teams enhanced and expanded key services and resources for researchers:
- The CTSI Recruitment Center launched to provide coordinated resources, services and consultations to facilitate cohort identification and the recruitment of research participants.
- Mirroring UF’s growth in clinical trials volume — which has more than doubled since 2012 — the Clinical Research Center continued a trend of annual growth in patient visits and protocols. Outpatient visits for 2016 are projected to surpass 5,500, an increase of 21 percent from 2015. The number of protocols increased by 23 percent, with more than 150 protocols active in 2016 — including more than 60 studies involving other Clinical and Translational Science Award institutions.
- To help meet growing demand, CTSI investigational pharmacy services expanded to include compounding and dispensing of biological and gene therapy products, as well as the ability to distribute to research pharmacies across the state.
- The Center for Cellular Reprogramming received an NIH R24 award to establish a Pharmacogenomics iPSC Library and Service resource, and initiated linkage with the newly funded CTSA iPSC Network.
Pilot Support: The CTSI and its programs supported six competitive pilot mechanisms to seed the growth of multidisciplinary investigator-initiated translational research at UF. CTSI-affiliated pilot programs received more than 100 applications and made 35 awards to support projects led by investigators in 10 colleges.
Translational Workforce Training and Education
The CTSI Translational Workforce Development Program built significant momentum in 2016 to advance its goal of leveraging the institute’s leadership, infrastructure, program models and faculty expertise to become a universitywide hub catalyzing new opportunities in translational science graduate education and training. The K College, T Team and F Force concepts have grown to support and convene more than 180 fellows and junior faculty as well as T and F award directors and trainees spanning multiple colleges. New K Awards at UF increased from six to seven per year in 2013-2015 to 14 in 2016, and T32 grants increased from nine in 2014 (supporting 38 predocs and 25 postdocs) to 16 in 2016 (60 predocs and 25 postdocs).

In 2016, the CTSI supported approximately 49 faculty members and trainees across its KL2, TL1, TRACTS and Mentor Academy programs. New programs launched include several diversity initiatives as well as a master’s program in biomedical informatics, with a PhD program in biomedical informatics approved to launch in Fall 2017. In the applied biotech training arena, Arizona became the second state to adopt the Biotechnician Assistant Credentialing Exam developed by the CTSI’s Biotility program.
Learning Health System Initiatives
The past year yielded progress across multiple initiatives designed to strengthen the capacity of UF’s learning health system environment:
Precision Medicine: The UF Health Personalized Medicine Program continued to develop, implement, study and refine methods that allow genetic information to be used as a routine part of patient care. CTSI resources facilitated the launch of a project at UF Health Jacksonville to study a point-of-care pharmacogenetics testing approach to guide clopidogrel therapy for heart stent patients, as well as development of a project to study genomic-assisted proton pump inhibitor use in GI clinics. The program also presented findings from a multisite analysis that showed CYP2C19 genetic testing at seven IGNITE sites significantly reduced the risk of cardiovascular events for heart stent patients with a genetic deficiency.
Translational Pilots: CTSI supported four new projects through its NIH-funded Translational Pilot Program and released a 2017-18 RFA with a focus on learning health system approaches that emphasize engagement of clinicians and integration of translational research into the clinical environment. The CTSI also conducted a survey of UF Health clinicians to assess opportunities and barriers to clinician participation in research.
Quality Improvement Registry: In collaboration with UF Health’s Office of Clinical Quality & Patient Safety, CTS-IT developed the UF Health Quality Improvement Project Registry and CQI Approver, scheduled to deploy in 2017. The CTSI envisions the registry will become a major resource to inform process-improvement pilots. In addition, the CQI Approver app will help streamline approval workflows through an algorithm that notifies users of project approval, incomplete requirements or IRB protocol requirements.
Integrated Data Repository and Consent2Share: The Integrated Data Repository continued to expand, with 5,341 queries in 2016 and data representing more than 830,000 patients. IDR data includes whether patients have agreed to participate in Consent2Share, which offers UF Health patients an opportunity to allow UF researchers to contact them about research studies for which they might be eligible based on information in their electronic health record. Close to 30,000 patients have enrolled to date through internal medicine and medical specialties, family practice, cardiovascular and pediatric clinics, with ongoing expansion underway.
Patient-Reported Outcomes: CTSI Biomedical Informatics Program faculty are collaborating with UF Health IT, Epic, Cerner and nine other universities to integrate patient-reported outcomes into electronic health record workflow as part of an NIH CTSA Collaborative Innovation Award led by Northwestern University.
Statewide and National Collaborations
CTSI made significant strides in expanding statewide and national collaborations to amplify the collective impact of translational research for the state and nation:
OneFlorida: As the coordinating center for the OneFlorida Clinical Research Consortium, the CTSI bridges two national research networks: the CTSA consortium and PCORnet. The OneFlorida consortium facilitated approval of 11 studies through the OneFlorida IRB, supported nine active studies and created the OneFlorida Data Trust, which was approved by the Patient-Centered Outcomes Research Institute as “research ready” and contains claims and electronic health record data for more than 10 million patients.
Community Engagement: HealthStreet celebrated its fifth year at UF and expanded its outreach to encompass more than 20 counties, with more than 8,400 HealthStreet members enrolled since 2011. HealthStreet faculty collaborated with four CTSA hubs to publish results of the CTSA Trust Project and with 21 CTSA hubs to develop the Our Community, Our Health town hall series as a multisite forum to engage researchers and community members in open dialogue.
Multisite Studies: The CTSI engaged a multisite team to help implement IRB, contracting and site initiation for a UF-led $15 million PCORI randomized pragmatic clinical trial at 45 institutions, and it assembled a liaison team to facilitate UF participation in the new CTSA Trial Innovation Network. CTSI investigators also are leading a CTSA Child Health Acceleration through a Multisite Planning, or CHAMP, pod project focused on screening for adverse childhood experiences in primary care settings.
Institute for Child Health Policy
Director: Betsy A. Shenkman, Ph.D.
 Building on nationally recognized research programs in pediatric quality of care, life-span research and biomedical informatics, the Institute for Child Health Policy, or ICHP, continued to carry out its mission to improve children’s health through innovative research and to serve as a transdisciplinary hub of child health research at UF and around the country.
Building on nationally recognized research programs in pediatric quality of care, life-span research and biomedical informatics, the Institute for Child Health Policy, or ICHP, continued to carry out its mission to improve children’s health through innovative research and to serve as a transdisciplinary hub of child health research at UF and around the country.
Using Biomedical Informatics to Improve Pediatric Quality of Care
As data analytics takes on an increasingly important role in health research and care delivery, ICHP faculty are leveraging big data to promote pediatric safety and quality of care. For example, in addition to evaluating quality and outcomes of care for children in Florida and Texas Medicaid programs, Betsy Shenkman, Ph.D., is using health care claims and electronic health record data from the OneFlorida Clinical Research Consortium to test and implement new pediatric quality measures developed by the Pediatric Quality Measures Program Centers of Excellence. With $675,000 in initial funding from the Agency for Health Care Research and Quality, Shenkman will lead a team of UF Health researchers and national collaborators with PCORI’s PedsNet and the Children’s Hospital of Philadelphia to evaluate two quality measures: preventive oral health care, and the safe and judicious use of antipsychotic medications. UF is one of only six institutions nationwide to participate in the PQMP.
Other ICHP collaborations in this field of research include:
- With funding from PCORI, ICHP researchers and the OneFlorida Clinical Research Consortium will collaborate with the Cincinnati Children’s Hospital Medical Center, a network member of PedsNet, to use electronic health record data to improve patient safety for those with sickle cell anemia and other childhood conditions.
- Mildred Maldonado-Molina, Ph.D., is collaborating with ICHP, the UF Family Data Center and the Florida chapter of the March of Dimes to map premature births in Florida’s 67 counties to help state policy-makers target areas with the highest needs.
- Amanda Hicks, Ph.D., has participated in national work to develop a terminology to examine adverse events in pediatrics. This groundbreaking work, published in Pediatrics, provides scientists and clinicians with an important tool to improve patient safety and quality of care.
- Betsy Shenkman, Ph.D., began serving as national co-chair of the Patient-Centered Outcomes Research Institute’s Pediatric Collaborative Research Group in 2016, working with leading child health researchers to help shape a national child-health research agenda for PCORI that includes a focus on biomedical informatics.
Promoting Health Across the Life Span
ICHP researchers are collaborating with scientists at UF in the department of pediatrics and the UF Diabetes Institute and nationwide to conduct vital research across the life span, as well. Collaborative research groups with PCORI and PedsNet are focusing on diabetes, obesity and cardiovascular health. In another project funded by UF’s Clinical and Translational Science Institute, Lindsay Thompson, M.D., M.S., assistant director of clinical research at ICHP, has partnered with four other CTSIs to lead a national initiative for the Child Health-Research Acceleration Through Multisite Planning, or CHAMP, program to accelerate research on screening for adverse childhood experiences in the primary care setting.
William Hogan, M.D., M.S., an ICHP professor and director of biomedical informatics at the UF CTSI, received a grant from PCORI to enhance and accelerate surveillance of congenital Zika syndrome using electronic health records and administrative data from PCORnet and the U.S. Food and Drug Administration’s Sentinel Initiative.
Chris Delcher, Ph.D., received a three-year, $196,248 grant from the Department of Justice to evaluate the Florida Prescription Drug Monitoring Program and track high-risk groups, such as women of reproductive age who use opioids and adolescents prescribed stimulants for ADHD.
Stephanie Staras, Ph.D., and Robert Lawrence, M.D., in the department of pediatrics, received a two-year Pfizer grant to study a school-based immunization program for meningitis Group B (Men B), in collaboration with the county health department, area public schools and the University of Florida.
ICHP Associate Director Matthew Gurka, Ph.D., is working with Josef Neu, M.D., in the department of pediatrics on a recently funded R21 from the National Institute of Child Health and Human Development to evaluate the effects of early antibiotic use on the developing intestinal microbiome and metabolome in preterm infants.
With a $45,000 grant from the national T1D Exchange Clinic Network, Ashby Walker, Ph.D., is working with Desmond Schatz, M.D., medical director of the UF Diabetes Institute and immediate past president of the American Diabetes Association, to develop a program in which UF college students mentor children with diabetes from low-income families.
Ramzi Salloum, Ph.D., and Lindsay Thompson are collaborating on a project to identify children most likely to start using tobacco products and to implement interventions to prevent that use.
Francois Modave, Ph.D., is working with Angelina Bernier, M.D., in the department of pediatrics to validate a fitness assessment and develop mobile health app for use by adults and children.
Advancing Health Care Research
ICHP researchers also are striving to improve the quality of child health research. For instance, ICHP biostatistician Keith Muller, Ph.D., and University of Colorado Denver co-principal investigator Deborah Glueck, Ph.D., received renewed NIH funding to continue offering their GLIMMPSE sample size-calculating software to researchers nationwide. The software helps calculate power and sample size for multilevel and longitudinal studies, typically used for following cohorts of children in nested relationships, such as schools or clinics.
Recognized Leaders in Child Health Research
ICHP researchers are nationally recognized and sought out for their expertise in quality of care, health disparities, data analytics, and health screening and promotion. Highlights from 2016:
- Matthew Gurka was elected to the Society for Pediatric Research for his outstanding contributions to pediatric research. Gurka also began a three-year term on the editorial board of The Journal of Pediatrics.
- William Hogan was elected to membership in the American College of Medical Informatics, one of the highest honors in this field.
- Michelle Cardel, Ph.D., gave a presentation on the social determinants of obesity in Hispanic adolescents at the National Academy of Medicine’s Obesity Interest Group.
- Dominick Lemas, Ph.D., was named one of 10 Keystone Symposia fellows, a two-year fellowship program for minority junior faculty funded in part by the National Institutes of Health.
- Stephanie Staras and Ramzi Salloum were named Cancer Fellows in the NCI’s Mentored Training for Dissemination and Implementation Research program, which trains researchers in methodologies to shorten the time it takes study findings to be incorporated into cancer treatments and prevention interventions.
- Ashby Walker began a two-year term on the American Diabetes Association’s National Health Disparities Committee, which helps the ADA reduce inequities facing populations disparately affected by diabetes.
In addition to providing a collaborative space for child health researchers across UF’s campus, the institute’s faculty members have expanded their diverse funding portfolio with the department of health outcomes and policy to garner $34.5 million in new grant funding in fiscal year 2015-16, for a total active portfolio of $94.3 million to fund life span research. ICHP faculty also continued to increase their research productivity, with 114 publications in the past fiscal year.
The UF Diabetes Institute
Director: Mark Atkinson, Ph.D.
 The UF Diabetes Institute completed its second year in 2016, pushing forward toward its overarching mission to see a diabetes-free world.
The UF Diabetes Institute completed its second year in 2016, pushing forward toward its overarching mission to see a diabetes-free world.
With one new person diagnosed with diabetes every 23 seconds and approximately one quarter of patients admitted to a UF Health Shands hospital having diabetes as part of their medical diagnosis, our mission is increasingly urgent.
Two words come to mind for the UF Diabetes Institute for 2016: growth and collaboration. This past year marks continued growth for some of UF’s hallmark diabetes programs, as well as new collaborations for future programs. While many notions could be highlighted, below are a represented selection from a program dedicated to research, improved patient care, training and public outreach, for which we at UF are proud to be a part.
Research and Training
Most people are aware of the importance of the heart, brain and lungs, but the pancreas is one of the human body’s most often forgotten organs. That is, unless it isn’t working. The UF Diabetes Institute is helping to grow a strategic, collaborative effort focused on pancreas research at the University of Florida. So much so, we now think of ourselves as “Pancreas U.” In addition to having been the coordinating center for the JDRF’s nPOD, the Network for Pancreatic Organ Donors with Diabetes, for almost a decade, multiple programs recently funded by the National Institutes of Health and the Helmsley Charitable Trust will increase UF’s leadership in this area (Drs. Mark Atkinson, Todd Brusko, Martha Campbell-Thompson, Clayton Mathews, Desmond Schatz and Cherie Stabler). This will also include developing a “pancreas atlas” that will, in detail, describe how the pancreas develops from birth through 10 years of age. Dr. Martha Campbell Thompson received an NIH Stimulating Peripheral Activity to Relieve Conditions, or SPARC, award to better understand neural networks in the pancreas. Beyond this, UF was one of 10 centers in the U.S. selected by NIH to study relationships between chronic pancreatitis, diabetes and pancreatic cancer (Drs. Christopher Forsmark, Kenneth Cusi and Steven Hughes). These programs account for well over $40 million in funding invested in pancreas-related research in the last decade that engages multiple colleges and disciplines at UF.
- The University of Florida remained the world’s top recipient of research funding from JDRF, which is the largest non-governmental entity providing funds dedicated to type 1 diabetes. Indeed, our university receives nearly 10 percent of the annual research funding from this international organization.
- The UF Diabetes Institute has grasped our institution’s challenge to increase its number of NIH grants dedicated to training. This past year saw numerous new NIH training awards, including an interdisciplinary T32 grant dedicated to training young investigators in the areas of diabetes and biomedical engineering as well as two new awards targeting diversity (F31 award).
Clinical Care
- The number of visits of patients with diabetes in UF Health Shands Hospital has increased tenfold over the past five years, from roughly 400 patients in 2011 to more than 4,000 in 2016. Dr. Kenneth Cusi, chief of the division of endocrinology, diabetes and metabolism in the UF College of Medicine’s department of medicine, has led the charge to continue to improve comprehensive diabetes care at UF Health.
- The pediatric endocrinology and diabetes program, led by Michael Haller, M.D., is the highest-ranking program in pediatrics or adult medicine at UF and of its kind in the Southeast by U.S. News & World Report.
- In like form, for the first time in recent history, UF’s adult endocrinology and diabetes moved into a position of national ranking in the 2016 U.S. News & World Report’s analysis of adult medical programs.
Outreach and Involvement
- In order to engage internal stakeholders in the strategic development of the UF Diabetes Institute, we held more than 100 meetings in the first quarter of 2016 in addition to a “collision breakfast,” which sparked collaborations between investigators that continue to showcase opportunities for interdisciplinary projects.
- Desmond Schatz, M.D., served as the 2016 American Diabetes Association President, Medicine & Science, and delivered a challenge to his peers during his keynote address at the ADA 76th Scientific Sessions to elevate diabetes to a top priority in government and society.
- Ashby Walker, Ph.D., was appointed to the American Diabetes Association’s National Health Disparities Committee, bringing her extensive expertise in disparities in Type 1 diabetes.
- The UF Diabetes Institute hosted its first 5K and Family Day, bringing together more than 200 patients, families and community members for an active day on campus.


- November is an awareness month for diabetes, so the UF Diabetes Institute led its first “Bluevember” campaign (including lighting of the Century Tower on campus and a photo contest for children with diabetes, the winning entries shown below), and increased regular community glucose screenings, and also hosted a World Diabetes Day event, engaging members of the university and Gainesville communities. Mark Atkinson, Ph.D., gave a keynote talk for World Diabetes Day that was viewed thousands of times.
- The Diabetes Institute began administrating Walk Alachua County, a weekly wellness walk program focused on reducing obesity and improving healthy lifestyles in the greater Alachua County community.
Additional Health Science Center Highlights
The UF Diabetes Institute is connected with more than 200 affiliate members across the university, and therefore the breadth of diabetes research that could be highlighted is immense. Here is a brief snapshot of recent research in the areas of diabetes prevention and treatment at UF:
- In collaboration with the College of Nursing, the UF Diabetes Institute is supporting an emerging program led by Lisa Scarton, R.N., Ph.D., focused on developing a working group to address health disparities related to type 2 diabetes in Native American populations in Florida.
- Michelle Cardel, R.D., Ph.D., and her team are developing an application geared toward helping patients with obesity and type 2 diabetes.
- David Janicke, Ph.D., conducted a major study that found that hungry parents may feed their kids larger portions of food.
- Arch Mainous, Ph.D., examined the relationship between handgrip strength and diabetes and hypertension in healthy weight adults.
- The results of a three-year clinical trial led by Kenneth Cusi, M.D., found that the drug pioglitazone is safe and effective in certain patients who have NASH, or nonalcoholic steatohepatitis, a chronic liver disease caused by fat buildup. Fatty liver disease is a risk factor for type 2 diabetes, even in non-obese patients.
Emerging Pathogens Institute
Director: J. Glenn Morris, M.D.
 The beginning of 2016 brought with it news of the devastating impact the Zika virus was having on newborns in South America, with the World Health Organization declaring the epidemic a “Public Health Emergency of International Concern.” In response, the Emerging Pathogens Institute ramped up its ongoing studies of arboviral infections, including Zika, initially allocating existing resources and then extramural grant funding toward understanding the virus and its transmission within Florida and the Caribbean. At the same time, EPI has continued to build its research portfolio in emerging pathogens/infectious diseases, further enhancing UF’s reputation as a top national and international center for infectious disease research. In the aftermath of Zika fever and Ebola, there has also been a strengthened emphasis on global health, reflecting the importance to Florida and the United States of understanding why pathogens emerge and are transmitted across the globe. Selected 2016 activities include the following:
The beginning of 2016 brought with it news of the devastating impact the Zika virus was having on newborns in South America, with the World Health Organization declaring the epidemic a “Public Health Emergency of International Concern.” In response, the Emerging Pathogens Institute ramped up its ongoing studies of arboviral infections, including Zika, initially allocating existing resources and then extramural grant funding toward understanding the virus and its transmission within Florida and the Caribbean. At the same time, EPI has continued to build its research portfolio in emerging pathogens/infectious diseases, further enhancing UF’s reputation as a top national and international center for infectious disease research. In the aftermath of Zika fever and Ebola, there has also been a strengthened emphasis on global health, reflecting the importance to Florida and the United States of understanding why pathogens emerge and are transmitted across the globe. Selected 2016 activities include the following:
- Zika has been a major focus for EPI throughout 2016. EPI created and moderated the UF Zika Working Group, which brought together scientists, clinicians and public health specialists from across the UF campus (and the county and state departments of health) to exchange information and facilitate the development of collaborative research programs. EPI and other UF scientists provided a special briefing on Zika for the Florida congressional delegation, and took a leadership role in speaking and other educational activities across the state. On the research front, Dr. John Lednicky, of the College of Public Health and Health Professions, and colleagues published an article in PLOS Neglected Tropical Diseases in April 2016, reporting initial identification and genetic characterization of the Zika virus in Haiti in 2014, “resetting the clock” for our understanding of the origin and spread of the virus. As the year progressed, EPI investigators were responsible for a series of publications describing clinical, genetic and transmission data for Zika. Starting with no Zika grant support at the beginning of the year, EPI investigators subsequently received major Zika-related funding from the NIH, the European Union, the National Science Foundation, the U.S. Department of Agriculture and the Department of Defense. Of particular note: in December 2016, UF/EPI, under the leadership of Dr. Rhoel Dinglasan at the College of Veterinary Medicine, received a five-year, $10 million grant to create the CDC-funded Southeast Regional Center of Excellence for Vector-Borne Disease, one of five such CDC centers across the nation focused on Zika and other vector-borne pathogens.

- EPI continues to play a key role in the characterization and control of Ebola. In December 2016, Dr. Ira Longini, of UF’s College of Public Health and Health Professions and the College of Medicine, and colleagues published an article in The Lancet confirming that the rVSV-ZEBOV Ebola vaccine tested in the 2015 Ebola Ça Suffit! vaccine trial had 100 percent efficacy in prevention of the disease onset.
- EPI, building on teams of faculty and student collaborators from PHHP, COM, Vet Med, IFAS, Engineering and other colleges, has continued to enhance its research base in Haiti, permitting direct study of a number of tropical diseases (including multiple diseases for which Florida may be at risk). Current studies include work on vector-borne transmission and clinical characteristics of dengue, chikungunya and Zika virus (Drs. Beau de Rochars [PHHP], Okech [PHHP], Lednicky [PHHP], Salemi [COM] and others), multi-drug-resistant tuberculosis (Dr. Lauzardo [COM]), cholera transmission and evolution (Drs. Beau de Rochars [PHHP], Ali [PHHP], Johnson [COM], Salemi [COM], Morris [COM] and others), malaria (Drs. Okech [PHHP], Dame [Vet Med] and Canella [COM]), and sexually transmitted infections (Dr. Maurelli [PHHP]); these studies are linked with work on sanitation, water systems and nutrition. Of particular note, EPI investigators (Drs. Morris [COM], Ali [PHHP], Salemi [COM], Beau de Rochars [PHHP] and Kenah [PHHP]) received two NIH R01 awards in 2016 to continue current work with cholera in Haiti. As reported in The New England Journal of Medicine, EPI investigators (Drs. Morris [COM] and Longini [PHHP/COM]) played a key role in development of recommendations to the Haitian Ministry of Health and the WHO regarding widespread administration of cholera vaccine in the wake of the devastation caused by Hurricane Matthew.
- In August 2016, EPI sponsored the Eighth World Melioidosis Congress in Cebu City, the Philippines. The Congress drew over 200 participants from 21 countries, and highlighted the increasing global recognition of the disease, caused by Burkholdaria pseudomallei, which is associated with some 100,000 deaths/year. EPI has one of the top research programs in the world on Melioidosis, let by Drs. Schweizer [COM] and Tuanyok [Vet Med].
- In the Gainesville area, EPI continues to provide technical assistance for the school-based influenza immunization program, a model program recognized nationally that has resulted in influenza immunization rates (in past years) in excess of 50 percent of Alachua County students. School-based immunization rates declined precipitously this year, in response to removal of the live attenuated oral vaccine (FluMist) from the market; UF/EPI investigators (Dr. Ryan [COM]) are currently evaluating the impact of this decline. In other influenza-related work, Drs. Lednicky [PHHP] and Iovine [COM] and colleagues have continued to evaluate the impact of genetic drift on clinical characteristics of influenza patients at UF Health Shands Hospital and in the community.
- A number of new faculty members joined EPI during 2016: These include Dr. Ilaria Capua, D.V.M., Ph.D. [IFAS], a virologist and veterinarian internationally recognized for her work with avian influenza — and a former member of the Italian Parliament — who is assuming leadership of the UF OneHealth program. Dr. Rhoel Dinglasan, Ph.D., M.P.H., M.Phil. [Vet Med], a UF preeminence scholar, comes from the Johns Hopkins Bloomberg School of Public Health, bringing expertise in malaria and arboviral research; as noted above, in December 2016 he received a five-year, $10 million grant to lead the CDC Southeast Regional Center of Excellence for Vector-Borne Disease. Dr. Eric Nelson, M.D., Ph.D., has come to EPI from Stanford University, bringing his expertise cholera transmission and pediatrics in Bangladesh and India. He is a recipient of the NIH Director’s Early Independence Award to develop mobile technology to provide clinical decision-support during cholera outbreaks, and answer fundamental basic-science questions about the progression and transmission of cholera.
Reflecting the diversity of research at EPI, a selection of other 2016 publications from EPI investigators includes: Identification and characterization of cefotxime-resistant bacteria in beef cattle (Dr. Jeoung [IFAS] and colleagues); Genomic epidemiology of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit (Dr. Salemi [COM] and colleagues); Vaccination with a ΔnorD ΔznuA Brucella abortus mutant confers potent protection against virulent challenge (Dr. Pascual [Vet Med] and colleagues); Mayaro Virus in child with acute febrile illness, Haiti, 2015 (Dr. Lednicky [PHHP] and colleagues); Prevalence of Escherichia coli O157:H7 from house flies (Diptera: Muscidae) and dairy samples in North Central Florida (Dr. Mai [PHHP] and colleagues); Coinfection of California sea lion adenovirus 1 and a novel polyomavirus in a Hawaiian monk seal (Neomonachus schauinslandi) (Dr. Wellehan [Vet Med] and colleagues); Investigating Rare Risk Factors for Nipah Virus in Bangladesh: 2001-2012 (Dr. Kenah [PHHP] and colleagues); An insecticide resistance-breaking mosquitocide targeting inward rectifier potassium channels in vectors of Zika virus and malaria (Dr. Bloomquist [IFAS] and colleagues); and Namibian farmland cheetahs (Acinonyx jubatus) demonstrate seronegativity for antibodies against Bacillus anthracis (Dr. Blackmore [CLAS] and colleagues).
UF Genetics Institute
Director: Patrick Concannon, Ph.D.
 It has been another year of growth at the University of Florida Genetics Institute. During 2016, we welcomed additional faculty members, bringing the total to 245. UFGI members represent seven colleges and 51 academic departments. Over the year, they brought in $133 million in sponsored research support, filed 60 US patents and published 788 scholarly articles. Their work appeared in prestigious journals such as The New England Journal of Medicine, Science, Nature, and Nature Genetics.
It has been another year of growth at the University of Florida Genetics Institute. During 2016, we welcomed additional faculty members, bringing the total to 245. UFGI members represent seven colleges and 51 academic departments. Over the year, they brought in $133 million in sponsored research support, filed 60 US patents and published 788 scholarly articles. Their work appeared in prestigious journals such as The New England Journal of Medicine, Science, Nature, and Nature Genetics.
Mission
The aim of the UFGI is to promote excellence in the areas of genetics and genomics at the University of Florida by: 1) building community, facilitating collaboration and creating opportunities for intellectual exchanges among investigators working in diverse taxonomic systems but with a common set of approaches in genetics and genomics, 2) supporting recruitment and retention of outstanding faculty in the areas of genetic and genomics, 3) supporting graduate education in the areas of genetics and genomics and 4) enhancing the ability of researchers at the University of Florida to compete for multidisciplinary research grants in the area of genetics and genomics.
Education
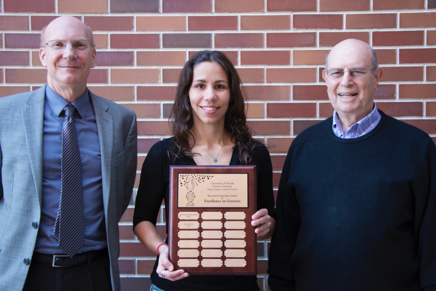 Our Genetics & Genomics Graduate Program has been a particular source of pride. Last year saw three students earn their doctoral degrees, bringing the total number of graduates to 23. Our intercollegiate program continues to grow, with seven more students admitted in the current year and interviews already underway for the class of 2017. Last year we introduced the Kenneth and Laura Berns Award for Excellence in Genetics. This year it was awarded to Lara Ianov, a Genetics & Genomics graduate student.
Our Genetics & Genomics Graduate Program has been a particular source of pride. Last year saw three students earn their doctoral degrees, bringing the total number of graduates to 23. Our intercollegiate program continues to grow, with seven more students admitted in the current year and interviews already underway for the class of 2017. Last year we introduced the Kenneth and Laura Berns Award for Excellence in Genetics. This year it was awarded to Lara Ianov, a Genetics & Genomics graduate student.
Our students have also been recognized by external organizations for their research. Ana Caroline Costa Sá received the American Society for Clinical Pharmacology and Therapeutics 2016 Presidential Trainee Award.
Outreach
The 2016 program of our annual cornerstone event, The Florida Genetics Symposium, was the most successful yet. Taking place Nov. 30-Dec. 1, 2016, more than 500 people registered to attend — the most participants in the history of the event. The conference featured nearly a dozen other distinguished speakers, from UF and from other institutions. Approximately 100 posters were presented, with student and postdoctoral associates receiving awards for best poster presentations.
As part of our collaborative efforts with innovative faculty at other institutions, we continued our weekly seminar series with presentations from 13 internal and external speakers. The invited speakers reflect the broad, multidisciplinary mandate of the UF Genetics Institute. The seminars included outstanding investigators from the fields of bioinformatics, genomics and cell biology working on a variety of species and model systems.
In August, UFGI hosted the third annual Phenotype Prediction Workshop. The objective of this workshop was to present recent results and theoretical developments of statistical models used to predict the phenotype of complex traits using genomic data. Presentations included studies from humans, trees, crops and livestock. The workshop attracted more than 100 on-campus participants, and was streamed live to over 300 online attendees from more than 30 countries.
 Other outreach endeavors included organizing the second UFGI DNA Day event on the UF campus. The April celebration featured activities and contests marking the anniversary of the elucidation of the structure of the DNA molecule. Over 100 students and faculty attended, including a visit from President Kent Fuchs.
Other outreach endeavors included organizing the second UFGI DNA Day event on the UF campus. The April celebration featured activities and contests marking the anniversary of the elucidation of the structure of the DNA molecule. Over 100 students and faculty attended, including a visit from President Kent Fuchs.
Institute on Aging
Director: Marco Pahor, M.D.
 The year 2016 was extremely successful regarding health care, education and research productivity. The Institute on Aging has expanded the health care and education venues, and has supported 53 extramural research grants through cores, pilots and mentoring, with a total cost of over $149.2 million, and $22.1 million in the 2016 annual period, which include major center grants, such as the Pepper Center, the P50 Sepsis project and the IOA contribution to the CTSI KL2 program, as well as large NIH-funded multicenter clinical trials, including the LIFE study, The Testosterone Trial, ASPREE, ENRGISE and the newly awarded MoTrPAC described below.
The year 2016 was extremely successful regarding health care, education and research productivity. The Institute on Aging has expanded the health care and education venues, and has supported 53 extramural research grants through cores, pilots and mentoring, with a total cost of over $149.2 million, and $22.1 million in the 2016 annual period, which include major center grants, such as the Pepper Center, the P50 Sepsis project and the IOA contribution to the CTSI KL2 program, as well as large NIH-funded multicenter clinical trials, including the LIFE study, The Testosterone Trial, ASPREE, ENRGISE and the newly awarded MoTrPAC described below.
Research
Pepper Center — The Claude D. Pepper Older Americans Independence Center (NIH P30AG028740; principal investigator, Dr. Marco Pahor) is completing its 10th year of funding and is poised to start the third five-year cycle after receiving an outstanding fundable score on the competitive renewal application. The center’s mission is twofold: 1) to optimize older persons’ physical performance and mobility through interdisciplinary approaches, and 2) to train new investigators in aging and disability research while developing their leadership qualities. Our goal is to enhance late-life health and independence, with a special focus on mobility. To accomplish our mission, our strategy is to attract studies and inventive investigators from diverse behavioral, clinical, basic and technological science disciplines with a common research focus: “mobility and prevention of disability.” Traversing the entire spectrum of biomedical investigation, including molecular biology, animal studies, clinical research, behavioral sciences, epidemiology and engineering, our research effort addresses the center’s general goal: to increase scientific knowledge that leads to better ways to maintain or restore independence of older people. The center trains Junior Scholars and supports investigators, resources, services, external studies, development projects and pilot/exploratory studies through seven integrated cores:
- Leadership and Administrative Core (Dr. Pahor);
- Research Education Core (Dr. Christiaan Leeuwenburgh);
- Pilot/Exploratory Studies Core (Dr. Christy Carter);
- Clinical Research Core (Dr. Stephen Anton);
- Metabolism and Translational Science Core (Dr. Leeuwenburgh);
- Biostatistics Core (Dr. Samuel Wu); and
- Data Science and Applied Technology Core (Dr. Todd Manini).
MoTrPAC. When we exercise, a cascade of benefits occurs, but researchers don’t know exactly what happens in the body to cause those benefits. Now, two separate teams at the University of Florida have received a portion of a $170 million push from the National Institutes of Health to discover the underlying mechanisms of exercise. For years, researchers have established that exercise is correlated with lowered risk of cancer, heart disease, stroke and diabetes and can help weight control. But how exercise impacts the body’s “molecular map” of proteins, peptides, circulating nucleic acids, lipids, hormones and other molecules is not well-understood.
The initiative, called Molecular Transducers of Physical Activity in Humans, or MoTrPAC, is a national research consortium that involves 25 universities and research centers across the country. Nineteen grants will support researchers across the country to collect samples from people of different races, ethnic groups, sex, ages and fitness levels. The samples will be analyzed to uncover how physical activity changes chemical molecules within the body, which could lead to people engaging in more targeted and optimized types of activity.
Dr. Pahor leads the consortium’s coordinating center (NIH U24AR071113) in conjunction with Wake Forest University and the University of Vermont, which will manage the development and implementation of the study’s protocols in both humans and animals. Researchers will examine the effect of exercise on humans both in the short term and over time. These experiments will be mirrored in animals at the initiative’s three preclinical animal study sites. Dr. Karyn Esser, Ph.D., associate program director of the UF Institute of Myology, is leading one of the MoTrPAC’s preclinical animal study sites.
These awards total approximately $170 million through fiscal year 2022. The awardees work as a consortium to develop plans for recruitment into clinical trials, identification of methods to analyze tissue samples and selection of animal models to best replicate human studies. The animal models will allow researchers to search for changes in tissues not easily accessible in human patients, such as the brain, lungs and kidneys.
Seven clinical centers across the country — six for adult participants, and one for those younger than 18 years of age — will recruit people from diverse racial and ethnic groups beginning in 2018. They will examine how molecular signals are altered following changes in exercise patterns. In addition to the clinical trial sites, MoTrPAC includes chemical analysis sites, three awards to conduct physical activity studies in animal models, a bioinformatics center to disseminate data and tools to the entire research community, and a coordination center to harmonize activities across the consortium. The program also provides funding to store data in a user-friendly public resource that any research can access to investigate the molecular mechanisms through which physical activity can improve or preserve health.
MoTrPAC is funded through the NIH Common Fund and managed by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute on Aging, and the National Institute of Biomedical Imaging and Bioengineering. Awards are made using the NIH Cooperative Agreement mechanism, which allows for substantial scientific interaction between the NIH and awardees.
The Testosterone Trial (NIH U01AG030644, UF principal investigator Dr. Pahor) — The primary results of this study were published in The New England Journal of Medicine in 2016. The major findings were that in symptomatic men 65 years of age or older, raising testosterone concentrations for one year from moderately low to the mid-normal range for men 19 to 40 years of age had a moderate benefit with respect to sexual function and some benefit with respect to mood, and depressive symptoms. Within the entire sample, there was a statistically significant increase in walking distance. Additional papers describing the results of these trials are currently in press at top journals, including JAMA.
The LIFE study (NIH U01AG022376, principal investigator Dr. Pahor) has continued to be highly productive in data analyses and publications, with over 75 papers published in peer-reviewed journals. The LIFE study has shown in a large multicenter trial that a structured physical activity program can prevent major mobility disability in sedentary older persons who are at high risk of disability. New analyses in LIFE published in the Annals of Internal Medicine have shown that physical activity reduced the burden of major mobility disability for extended periods, through enhanced recovery and diminished risk for subsequent disability, and that the intervention is cost-effective.
Nutritional and Pharmacologic interventions. We currently have a number of ongoing pharmaceutical and/or nutritional interventions, including a multi-site clinical trial investigating the effects of the angiotensin receptor blocker losartan and omega-3 polyunsaturated acids ω-3) as fish oil in reducing low-grade chronic inflammation and improving walking ability in older adults with elevated levels of inflammation (NIH U01AG050499 — ENabling Reduction of low-Grade Inflammation in Seniors [ENRGISE]; Dr. Pahor, principal investigator, Dr. Manini, site principal investigator). Study-wide, to date we have recruited over half of the target sample of 300 older adults who are at risk of mobility decline. Anticipated completion of recruitment is April 2017.
We also have an active R01-funded clinical trial investigating the effects of resveratrol on mitochondrial function and mobility (NIH R01AT007564 — Resveratrol to enhance vitality and vigor in elders [REVIVE]; Dr. Anton, principal investigator). This study uses a prospective, parallel design to determine whether 90 days of resveratrol supplementation in older men and women (≥ 70 years) is associated with 1) increases in muscle mitochondrial respiration, 2) increases in levels of PGC-1α, AMP-activated protein kinase (AMPK) and sirtuins (SIRT1 and SIRT3), and 3) improvements in functional performance and metabolic parameters. To date, we have recruited approximately half of the target sample of 60 moderate- to low-functioning participants who are randomized to receive a placebo (n=20), 1,000 mg/day of resveratrol (n=20), or 1,500 mg/day of resveratrol (n=20) for a 90-day period. Muscle specimens from the vastus lateralis are collected at baseline and 90 days for biochemical analyses of the primary outcome of mitochondrial function.
Metabolism and Translational Science Core. The Claude D. Pepper Older Americans Independence Center (NIH P30AG028740) Metabolism and Translational Science Core conducts translational research with biomarkers to determine mechanisms of age-related mobility loss (core leader, Dr. Leeuwenburgh). The Core supports studies on aging; surgical procedures and muscle disuse; diabetes; osteoarthritis; obesity; nutrition; and aging as it relates to cognition, sepsis and HIV — all linked to the current center cycle’s focus: “prevention of disability and improvement of mobility.” This Core has been exceptionally productive, having contributed to over 220 published papers between 2010 and 2015 and having collaborated on over 65 grants. This past year (2016-2017) this Core is involved with over 25 active grants on which it is performing analysis. This Core also closely works with 10 of the current and previous Junior Scholars and five external investigators on research projects.
Health Care
Our clinical practice (chief, Dr. Laurence Solberg) continues to grow, with increased numbers of patients, providers and clinical venues. We recruited physicians and physician extenders to our clinical team to expand our presence in the outpatient clinic, the hospital and community skilled nursing facilities.
The Geriatrics Consult service in the UF Health Shands hospital added a physician assistant to assist in handling the increased demand for geriatrics input into the care of older hospitalized patients. Using the “embedded geriatrician” model we established the benefits of the Geriatric Consult services in partnering with the Medical and Surgical services to better serve our older patients. We continue to make a difference in the emergency room, with our geriatrician available to consult in the E.R. to intervene early in the care of geriatric patients.
We have successfully implemented our model of the “embedded geriatrician” in two of the local skilled nursing facilities and now with the addition of our PAs to the Skilled Nursing Facility team we have a geriatrics provider on site at the facility every week day. By being more involved in the care of the patient during rehabilitation, and having a greater presence in the facility, we have decreased readmissions to the hospital. Using this model in the rehabilitation centers, we were able to increase the amount of short-term rehabilitation beds available to our patients and increase the continuity of care we provide by being able to better understand the hospitalization and to continue the work of the geriatrics consult team management to aid in the recovery and return to independence of our patients.
In our practice we place major emphasis on quality of life and maintaining functional ability to be independent longer. We initiated a sarcopenia or frailty screening into our clinic visits in the UF Health Senior Care practice. This screening, consisting of tracking gait speed, grip strength and weight loss, along with our previously implemented clinical frailty score, allows us to identify older people at risk for becoming frail and allows us the ability to intervene. Our interventions range from participation in a clinical study on mobility or exercise to physical therapy for strength or gait training. By translating our research to clinical care, we are able to identify those patients at risk for losing physical strength, functional abilities and independence and make a difference before it affects their lifestyle.
Education
Medical Education. (chief, Dr. Laurence Solberg) Our revisions of the Geriatric Medicine rotation for fourth-year medical students continues in our four-week mandatory rotation. The rotation, which includes geriatric medicine, palliative care and geriatric rehabilitation medicine, now has a redefined assessment tool that aligns with the Association of American Medical Colleges and American Geriatrics Society medical student competencies in geriatrics. We continue to use our highly successful experiences including simulation exercises with standardized patients in an observed patient encounter focusing on the issue of polypharmacy in the elderly, a virtual dementia experience and visits with home hospice teams visiting patients in their home environments. Students have options to participate in more than 10 different clinical sites to gain the experience of following patients in a variety of care settings that are encountered by geriatric patients.
Research Education Core. The Pepper OAIC Research Education Core (NIH P30AG028740; core leader, Dr. Leeuwenburgh) promotes the development of independent investigators in interdisciplinary research on aging related to older Americans’ mobility. This past year we have already graduated four out of the seven Pepper Scholars because of either obtaining independent funding and/or promoted in their academic career. Within this core we have the K-College attended by early career investigators, including postdoctoral fellows who are invited to a monthly luncheon seminar. The current listserve of attendees includes about 110 early career Scholars, with 40 to 50 attending the seminars on a monthly basis. Topics presented are relevant to early career faculty, and these range from life-work balance to UF core facilities available to Scholars at the Pepper Center and CTSI. This also provides peer support and opportunities to raise issues of concern or discuss need for resources. This vore organize highly interactive sessions in which individual scholars can present progress or issues for discussion related to experimental design, issues related to IRB and other research- or academically oriented issues. Scholars can also participate on writing a K or R-type grant, in the K2R Boot camp. This Boot camp features the “flipped classroom” approach, using grant writing video lectures and other material available online, with eight monthly sessions in which participants bring their completed grant application sections for critique and questions. This culminates in three monthly sessions of mock study sections in which faculty and Scholars review the grant application in the presence of other Scholars and mentor(s) with written critiques made available prior to the grant submission deadline.
Graduate Education. (committee chair, Dr. Christy Carter) More than 10,000 baby boomers turn 65 every day, and according to the Eldercare Workforce Alliance, the United States is ill-prepared to meet current and future workforce needs for its aging adult population. The UF IOA provides a solution to this major problem by offering an online master’s degree in gerontology or graduate certificate in aging and geriatric practice. Since 2014 our online graduate programs have targeted working health care professionals to provide them with an asynchronous learning experience, designed to fit their busy schedules. We offer 10 courses ranging from the basic biology of aging, geriatrics and age-related diseases, clinical neuroscience to the basics of research and epidemiology. Courses are designed and taught by our expert faculty, based upon their own research to provide practical knowledge that students may put directly to practice. Our student body continues to grow and is highly diverse. Enrollees are professionals working in a variety of fields, including physicians, nurses, psychologists, directors of assisted living facilities, law enforcement officials and policy makers. A large majority of our students reside in the Southeast; however, we are increasingly receiving enrollments from all over the country and Puerto Rico. We also serve local UF graduate and medical students who are interested in supplementing their own curriculum to specialize in gerontological studies. In addition, our faculty participate as educators and mentors in several Ph.D. programs throughout UF’s academic health center and the university at large, including Biomedical Sciences, Psychology, Nursing, Public Health, Pharmacy, and Health and Human Performance.
Evelyn F. & William L. McKnight Brain Institute
Director: Todd Golde, M.D., Ph.D.
 The Evelyn F. and William L. McKnight Brain Institute of the University of Florida initiated a new era with the appointment of Todd Golde, M.D., Ph.D., as executive director effective Dec. 1, 2016. Dr. Golde, a professor of neuroscience in the UF College of Medicine, established and was the inaugural director of the Center for Translational Research in Neurodegenerative Disease at UF. Steven T. DeKosky, M.D., who served as interim director of the MBI for the majority of 2016, will remain active in the MBI as deputy director. Both Drs. Golde and DeKosky look forward to working closely with the multiple neuroscience and neuromedicine research communities at UF. Gathering input from the numerous stakeholders on the UF campus during the coming year, they will develop a strategic plan for the Brain Institute that they hope will further enhance and build upon the impact and visibility of neuroscience research conducted at UF.
The Evelyn F. and William L. McKnight Brain Institute of the University of Florida initiated a new era with the appointment of Todd Golde, M.D., Ph.D., as executive director effective Dec. 1, 2016. Dr. Golde, a professor of neuroscience in the UF College of Medicine, established and was the inaugural director of the Center for Translational Research in Neurodegenerative Disease at UF. Steven T. DeKosky, M.D., who served as interim director of the MBI for the majority of 2016, will remain active in the MBI as deputy director. Both Drs. Golde and DeKosky look forward to working closely with the multiple neuroscience and neuromedicine research communities at UF. Gathering input from the numerous stakeholders on the UF campus during the coming year, they will develop a strategic plan for the Brain Institute that they hope will further enhance and build upon the impact and visibility of neuroscience research conducted at UF.
Neuroscience and neuromedicine research continue to flourish and expand at UF. The current NIH portfolio of neuroscience grants exceeds $35 million a year, with more than 100 NIH-funded grants along with numerous state of Florida and private foundation grants. Both the departments of neuroscience (2016 ranking, No. 12) and neurosurgery (2016 ranking, No. 15) are among the top-ranked UF College of Medicine departments in the NIH rankings from the Blue Ridge Institute for Medical Research. Although research is only one of the many factors that influence the national rankings, the growth of our neuroscience research supports both the visibility and perception of our clinical programs. Notably, in 2016 UF Health neuromedicine climbed 19 spots from the prior year to rank No. 21 in the country in the U.S. News & World Report rankings — making it one of the top two neuromedicine programs in the Southeast.
With an influx of new faculty in the neurosciences over the last five years, in part due to the UF preeminence initiative, a number of studies have coalesced that have resulted in major programmatic NIH funding. The 1Florida Alzheimer’s Disease Research Center, or ADRC, a P50 grant funded by the National Institute on Aging, is now in its second year of funding. It is one of only 30 NIH-funded ADRCs in the country; its unique focus on cognitive impairment in the elderly Hispanic population distinguishes it from the focus of the other ADRCs. Directed by Dr. Golde, the 1Florida ADRC represents a unique partnership with Mount Sinai Medical Center in Miami Beach, the University of Miami, Florida Atlantic University, and Florida International University and is the only federally funded ADRC in Florida. Serving as a hub for collaborative Alzheimer’s disease research, the 1Florida ADRC is already spurring exciting new research at UF and the other participating institutions.
Laura Ranum, Ph.D., who directs UF’s Center for NeuroGenetics, leads an NIH/NINDS (National Institute of Neurological Disorders and Stroke) Program Project Grant (P01) focusing on the central nervous system effects of myotonic dystrophy and molecular mechanisms underlying that disabling disease, which affects both neuromuscular function and cognition. These studies extend pioneering work led by Dr. Ranum demonstrating that microsatellite DNA repeats can be translated into peptides. This translation occurs despite the fact that these DNA repeats lack the canonical (required) signals for translation of proteins. Indeed, in part for recognition of this remarkable discovery, Dr. Ranum was appointed a fellow of the American Academy of Arts and Sciences, one of the highest honors in American sciences. Dr. Ranum and colleagues have also developed a novel mouse model of amyotrophic lateral sclerosis, or ALS, caused by a microsatellite repeat expansion in the C9orf gene, the most common of the several genes that cause ALS. This model is now being used to test novel therapeutic approaches to this form of ALS.
Dawn Bowers, Ph.D., of the College of Public Health and Health Professions, and David Vaillancourt, Ph.D., of the College of Health and Human Performance, co-lead an NIH-training grant (T32) on interdisciplinary training in movement disorders and neurorestoration. This training grant demonstrates the truly interactive nature of neuroscience research and training at UF as well as how focused translation research efforts can lead to the development of world-class programs. Students from engineering, neuroscience, applied physiology, rehabilitation and clinical and health psychology are being supported by the grant. The T32 involves more than a dozen faculty from multiple colleges and departments at UF. Indeed, the T32 leverages longstanding excellence in the Center for Movement Disorders and Neurorestoration led by Michael Okun, M.D., chair of the department of neurology, and Kelly Foote, M.D., a professor of neurosurgery. Their pioneering work in deep brain stimulation surgery was highlighted recently by National Geographic magazine. The T32 helps to solidify UF’s reputation as a leading institution for research on movement disorders.
Most recently, UF received a large multi-principal investigator NIH research (R01) grant. This five-year, $5.7 million grant, titled Augmenting Clinical Training in Older Adults: The “ACT Study,” is led by Adam Woods, Ph.D., Michael Marsiske, Ph.D., and Ronald Cohen, Ph.D., all now in the department of clinical and health psychology at UF’s College of Public Health and Health Professions and department of aging and geriatric research in the College of Medicine. Cohen and Woods are director and assistant director, respectively, of the Cognitive Aging and Memory Clinical Translational Research Program, or CAM-CTRP, one of two major programs supported by the McKnight Brain Research Foundation. This new translational grant aims to test the efficacy of a combination of methods designed to slow the process of age-associated memory loss — a major focus of the MBRF and CAM-CTRP — and potentially prevent onset of cognitive decline and dementia. The study will test how harmless low-voltage transcranial direct current stimulation, a form of noninvasive brain stimulation, can be combined with cognitive training to slow cognitive decline in the elderly. The ACT study can be attributed in large part to the ongoing support of UF and the MBI by the MBRF. The MBRF was established by Evelyn F. McKnight in 1999 and is responsible for the gift that named the McKnight Brain Institute of the University of Florida. In establishing the MBRF, it was Mrs. McKnight’s intent that it would support scientific research on the understanding and alleviation of age-related memory loss. Notably, the MBRF provides direct and ongoing support for both the UF CAM-CTRP program and the age-related memory loss program, which conducts studies in memory biology and behavior in animal models and translation.
The newly formed Center for Respiratory Research and Rehabilitation, housed in the MBI and led by Gordon Mitchell, Ph.D., a preeminence hire and a professor of physical therapy and neuroscience, had a very successful year. The CRRR submitted an institutional training grant application to the National Heart, Lung and Blood Institute to support the BREATHE Training Program (Breathing Research and Therapeutics). This application involves 62 trainers and collaborators from the academic health center, engineering and the applied physiology and kinesiology department. The grant received a score in the fundable range and, if not funded, this council will likely be funded upon resubmission. Members of the CRRR have been awarded a SPARC (Stimulating Peripheral Activity to Relieve Conditions) grant from the NIH Director's Common Fund titled: “Functional mapping of peripheral and central circuits for airway protection and breathing.” This grant, led by Don Bolser, Ph.D., a professor in the College of Veterinary Medicine, provides $2.65 million in total annual costs. Multiple MBI investigators are essential to the conduct of this grant (Drs. Mitchell, David Fuller, Ph.D., Elisa Gonzalez-Rothi, D.P.T., Ph.D., and Ronald Mandel, Ph.D.). Additional new recruits to UF participating in the CRRR include Erica Levitt, Ph.D., (pharmacology and therapeutics), Russ Hepple, Ph.D., (physical therapy) and Tanja Taivassalo, Ph.D., (physiology and functional genomics). The CRRR is a great example of how the MBI is not just about a building but about supporting programmatic activities that have campuswide reach.
These large programmatic grants speak to our successful efforts to build and support translational, thematic, team science within the MBI. However, the foundation of our neuroscience research activities remains the individual investigator-based awards — R01s, R21s, private foundations and state grants. One of the major hallmarks of success in building programmatic areas of research is to ensure that we not only attract and retain preeminent scientists, such as Gordon Mitchell (PHHP) and Carol Mathews, M.D., (COM, psychiatry), but also support the careers of the next generation of investigators. The success of our junior investigators and trainees over the last year in numerous programs and departments has been outstanding, and demonstrates how investment in programmatic activities can establish the MBI and affiliated departments and programs. Our success here is reflected in the granting of T32 NIH training awards. Examples of our junior faculty and trainee successes follow.
Led by Duane Mitchell, M.D., Ph.D., a professor of neurosurgery, the Brain Tumor Immunotherapy Program is funded in large part by the Lillian S. Wells Foundation and by matching funds from UF and the MBI. The BTIP is an outstanding example of how programmatic investment can provide great opportunities for new investigators to thrive. Dr. Mitchell was the first recruit to the program and has quickly established himself as a national leader in brain tumor immunotherapy. David Tran, M.D., Ph.D., Maryam Rahman, M.D., and Elias Sayour, M.D., Ph.D., recently appointed junior faculty in the department of neurosurgery, all have received NIH faculty career development (K) awards. Notably, all of their funded work is highly translational, and demonstrates the growing integration of our basic and clinical neuro-oncology research efforts. The success of the program and anticipated future growth will be an important part of the future efforts of the UF Cancer Center to obtain National Cancer Institute designation as a nationally designated (and quality) cancer center.
Another example of programmatic efforts enabling our young investigators is the aforementioned Age-Related Memory Loss Program. This program is led by Tom Foster, Ph.D., a professor of neuroscience, and like the CAM-CTRP has ongoing support from the MBRF. This program supports multiple investigators in preclinical studies of age-related memory loss. In 2016, Sara Burke, Ph.D., an assistant professor in the department of neuroscience, received three new R01 awards studying varying aspects of cognitive aging. Dr. Burke was also the recipient of an American Psychological Association Distinguished Scientific Contributions Award. Andrew Maurer, Ph.D., another recently appointed assistant professor in the department of neuroscience, also received his first R01 and has a second R01 scored in the range that it is almost certain to be funded. We are delighted by the success of our young MBRF-supported faculty.
A third example of programmatic efforts benefiting junior scientists comes from the Center for Translational Research in Neurodegenerative Disease. This center, established by Dr. Golde and now led by David Borchelt, Ph.D., a professor of neuroscience, focuses on understanding and finding new therapeutic approaches for neurodegenerative disorders such as Alzheimer’s, Parkinson’s disease, ALS and rare disorders that are thought collectively to be caused by excessive accumulation of different proteins in the brain. One of our recent M.D.-Ph.D. trainees, Amanda Sacino, was accepted into the neurosurgery residency program at The Johns Hopkins University, one of the top training programs in the country. Working in the laboratory of Benoit Giasson, Ph.D., a professor of neuroscience, Dr. Sacino published 10 manuscripts, including eight first-author manuscripts, during her graduate and medical training. Most of these studies centered on how pathology spreads in Parkinson’s disease, and these articles are having a significant impact on the field, having been collectively cited almost 300 times in the less than three years since they have been published. Dr. Sacino’s success in our neuroscience training program highlights not only how our junior faculty but also our trainees benefit by working in a translational research environment.
Numerous scientific advances have also emerged in the MBI programs. A number of these are highlighted in the Neuromedicine 2016 Progress Report (https://indd.adobe.com/view/12a0fdf8-db65-4bb5-a26f-9ba404bf46e1). Multiple neuroscience investigators (Drs. Adam Woods, Sara Burke, Brian Hoh, Edgardo Rodriguez, Mavis Agbandje-McKenna, Habibeh Khoshbouei and Eric Wang) have been featured in the UF Research Landscape videos, which can be found at http://med.ufl.edu/research/video-spotlights/. The report and these videos show snapshots of our diverse and growing neuroscience research portfolio. Over the next year the MBI will work with our stakeholders to create additional forums for highlighting our research advances. Indeed, the breadth of our neuroscience research at UF is impressive and we need novel and efficient ways to communicate our advances both internally and externally.
A number of new clinical investigators have been hired who will support translational neuroscience research efforts as well as the larger clinical mission that will be necessary to support the opening of the new UF Health Neuromedicine Hospital this December. Dr. Sri Gururangan, FRCP, was recruited from Duke University to lead the pediatric neuro-oncology program. Dr. Michael Jaffee, M.D., an associate professor of neurology and a 21-year veteran of the U.S. Air Force, brings experience from having served as national director of the Defense and Veterans Brain Injury Center and a wartime tour as chief of the medical staff at the main U.S. theater hospital in Iraq. An expert in traumatic brain injury, Dr. Jaffee was recruited to establish a multidisciplinary brain trauma clinic associated with our memory disorders and movement disorders clinics. Dr. Katharina Busl, M.D., now chief of UF neurocritical care, is a fellowship-trained neurointensivist from Harvard/Massachusetts General Hospital. She has appointments in neurology, neurosurgery, anesthesiology and bioengineering.
 We continue to update the MBI facilities and resources. The MBI’s Advanced Magnetic Resonance Imaging and Spectroscopy facility, part of the National High Magnetic Field Lab funded by the National Science Foundation, expanded both their human imaging capabilities and their support of preclinical research programs through instrument additions this year. A 3T Siemens Prisma scanner was installed in December 2016 to support a rapidly increasing number of federally funded UF investigators who are studying Parkinson’s disease, muscular dystrophy, aging and cognition, Alzheimer’s disease, adolescent brain cognitive development, traumatic brain injury and more. The Prisma has the strongest gradients available for human imaging, advanced motion correction algorithms and increased flexibility in scanning disparate areas (i.e., head to foot without having to change coils or having the subject get up and turn around). A new Bruker Advance console was installed in August to support preclinical applications at 11.1 T. It offers phased array imaging at micron resolution as well as in vivo spectroscopy methods for monitoring metabolites via 1H, 31P and 13C-DNP methods.
We continue to update the MBI facilities and resources. The MBI’s Advanced Magnetic Resonance Imaging and Spectroscopy facility, part of the National High Magnetic Field Lab funded by the National Science Foundation, expanded both their human imaging capabilities and their support of preclinical research programs through instrument additions this year. A 3T Siemens Prisma scanner was installed in December 2016 to support a rapidly increasing number of federally funded UF investigators who are studying Parkinson’s disease, muscular dystrophy, aging and cognition, Alzheimer’s disease, adolescent brain cognitive development, traumatic brain injury and more. The Prisma has the strongest gradients available for human imaging, advanced motion correction algorithms and increased flexibility in scanning disparate areas (i.e., head to foot without having to change coils or having the subject get up and turn around). A new Bruker Advance console was installed in August to support preclinical applications at 11.1 T. It offers phased array imaging at micron resolution as well as in vivo spectroscopy methods for monitoring metabolites via 1H, 31P and 13C-DNP methods.
The addition of the 3T scanner is essential for new translational research activities at UF. For example, Sara Jo Nixon, Ph.D., a professor of psychiatry, and Linda B. Cottler, Ph.D., M.P.H., chair of epidemiology, are part of the landmark Adolescent Brain Cognitive Development (http://www.abcdstudy.org/) study, and will study 400 adolescents from the North Central Florida region who will be scanned using this machine. UF is one of 21 research sites across the country following 10,000 children ages 9 and 10 year in a 10-year longitudinal study, the first of its kind to examine brain development and child health using advanced neuroimaging and bioassays in combination with assessments of cognition, environments, substance use and social function.
Overall, the AMRIS facility, led by Joanna Long, Ph.D., supports more than 60 grants and 10 clinical trials.
Due in large part to efforts of Dr. Habibeh Khoshbouei, Ph.D., Pharm.D., an associate professor of neuroscience, who was principal investigator on an NIH shared instrument grant, we have a Nikon multiphoton Super-Resolution Imaging System available in the Cell and Tissue Analysis Core in the MBI for all researchers. An example of an image obtained from this type of microscope is shown below. Instrumentation grants, like training grants, are large and complex endeavors, and typically provide only a minor return to the PI, but are invaluable for the institution and its researchers. We are extremely grateful to Drs. Khoshbouei, Bowers and Vaillancourt and all the investigators who helped with the submission of these successful grants and other T32 and instrument grants that hopefully will be funded in the future, for their efforts on behalf of UF and the MBI. Looking forward, we will continue to assess our equipment needs to ensure that our scientists are supported with cutting-edge instrumentation.
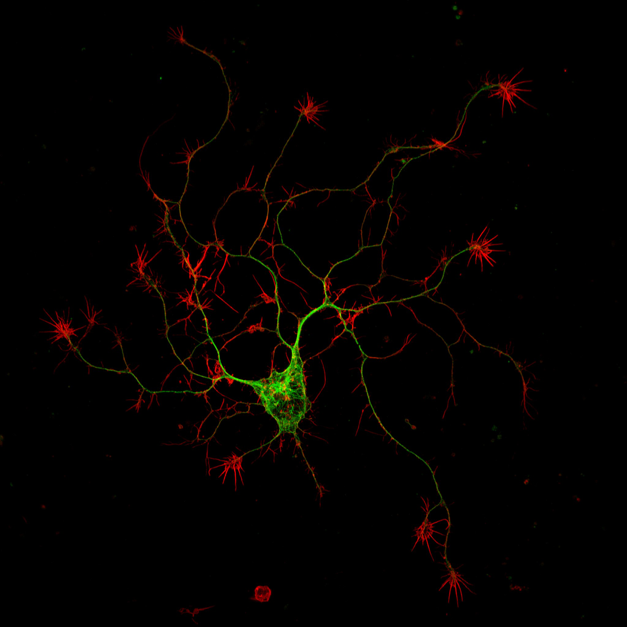
The MBI continues to support our training and education activities, and in the future we hope to support additional efforts to increase the awareness of our strengths in neuroscience research. This year the MBI launched a new Summer Neuroscience Internship Program. This program, designed to engage diverse undergraduate students in neuroscience research, was a tremendous success, with 10 undergraduates supported. The SNIP program was led by Sara Burke and Jada Lewis, Ph.D., from the department of neuroscience. The MBI also continued its support of Brain Awareness Week activities, including the fourth annual William G. Luttge Lectureship in Neuroscience, which was held March 14, 2016, with Carol Barnes, Ph.D., presenting. Dr. Barnes is the Regents’ Professor in the departments of psychology, neurology and neuroscience, and the Evelyn F. McKnight Endowed Chair for Learning and Memory in Aging, and director of the Evelyn F. McKnight Brain Institute in Tucson, Arizona.
The MBI also launched the MBI Neuromedicine Scholars program with Dr. Hank Paulson from the University of Michigan as our first Neuromedicine Scholar. This program was designed to support visits from eminent neuroscientists and opportunities not only for a seminar presentation but also for less formal interactions with trainees to provide both career and scientific advice. Further, it was designed to publicize our neuromedicine research programs. We think that this was a success, as Dr. Paulson’s parting words were, “Thanks for inviting me. This was great. I had no idea how strong the neuroscience research environment was here at UF.” We hope that with more activities like the Neuromedicine Scholars Program, we will continue to get the word out: neuroscience and MBI-supported programs are thriving at UF and we all should collectively be proud of our accomplishments in 2016.
UF Health Shands (Shands Teaching Hospital and Clinics Inc.)
CEO: Ed Jimenez, M.B.A.
 It’s been another outstanding year for the UF Health family and we’re thrilled to share the 2016 accomplishments from UF Health Shands. We owe all these successes to our staff of more than 9,000 employees and more than 3,000 volunteers, who dedicate themselves every day to serving our patients.
It’s been another outstanding year for the UF Health family and we’re thrilled to share the 2016 accomplishments from UF Health Shands. We owe all these successes to our staff of more than 9,000 employees and more than 3,000 volunteers, who dedicate themselves every day to serving our patients.
Clinical quality remains Job 1 as we continue to work together to deliver exceptional medical care, value and service to every patient at every encounter. In February, we formally rolled out Hospitality Huddles, twice-monthly briefings in which teams come together to discuss a specific Hospitality and Service standard of behavior. The goal is to personalize the standards, encourage staff to model them and ultimately make a positive difference for patients, visitors and each other. Staff and patients have already noticed — feedback seems to recognize that we’re more welcoming and attentive. Huddles are used across the organization by faculty, residents and volunteers who provide care and service at UF Health Shands, the UF Health Physicians practices and the UF College of Medicine. They’re making UF Health a better place to work and receive care.
Another win for quality care and service: The Efficiency, Effectiveness and Patient-Centeredness initiative, or EEPC, was recently launched by Dr. Guzick and Randy Harmatz, M.B.A., UF Health Clinical Quality and Patient Safety senior vice president and chief quality officer, as an interdisciplinary priority endeavor. This coalition of more than 250 executive faculty and administrative leaders, managers and frontline staff is now working to further boost clinical quality and the patient experience across the academic health center. They collaborate to address key quality measures like length of stay, patient-centeredness and community engagement.
It's always great to receive external validation for the outstanding work of our teams, recognizing our exemplary results on a national level. The 2016 U.S. News & World Report national rankings placed us in the top 50 of the Best Hospitals and Best Children’s Hospitals in 17 pediatric and adult specialties — the most of any hospital in Florida hospital.
In 2016, six UF Health Shands nursing care units had current Beacon Awards, a reflection of our nurses’ commitment to providing experienced care and expert caring. The Cardiac ICU, Pediatric ICU and Surgical/Trauma ICU teams each earned a gold-level Beacon Award for Excellence, while the Post Anesthesia Care Unit earned a silver-level Beacon Award. These awards come from the American Association of Critical-Care Nurses and are one of the highest honors in nursing.
![]()
The UF Health Shands Transplant Center and LifeQuest Organ Recovery Services celebrated 50th anniversaries in 2016. Our transplant teams have performed more than 8,300 transplants at UF Health Shands since achieving the state’s first adult kidney transplant in 1966. Beyond the numbers, each case is truly life-changing for our patients and families.
One of my favorite events of the year is the Milestone Service Awards Banquet, where we honor UF Health Shands employees who have achieved 10 or more years of service. Last spring, we celebrated nearly 800 employees, including many 30-, 35- and 40-year honorees, as well as a 45-year honoree.
Our reputation as an employer of choice continued to grow in 2016. UF Health was once again included on Forbes’ list of the America’s Best Employers, ranking 89th out of 500 companies. Meanwhile, Becker’s Healthcare named UF Health as one of the nation’s 150 great places to work in health care, and Becker’s Hospital Review named UF Health Shands Hospital as one of the 100 great hospitals in America.
As always, our expert physicians, nurses and clinical and support staff worked diligently as patient volumes continued to grow. Rising to the challenge, in fiscal year 2016 our teams managed 55,091 hospital admissions, 116,248 E.R. visits, 817,284 hospital-based outpatient visits and 6,193 UF Health ShandsCair emergency transports. Meanwhile, UF Health Physicians faculty practices tracked 858,922 outpatient visits. These impressive, sustained volumes across our clinical programs reflect the dedication of everyone in clinical and support roles.
We experienced another year of tremendous growth and expansion. Our teams made rapid progress on construction of the UF Health Heart & Vascular and Neuromedicine hospitals. With an average of 450 workers on site every day, this $415 million project is scheduled for completion in December. Hundreds of staff are participating in transition planning workgroups and leading this exciting endeavor.

Additionally, the UF Health Children’s Surgical Center opened to accommodate the growing need for specialized pediatric care; the fourth UF Health Pediatrics primary care practice opened at Tioga Town Center; the UF Health Shands Emergency Center at Kanapaha, our second freestanding E.R., opened; we completed Phase 1 of the Neonatal ICU expansion at UF Health Shands Children’s Hospital; and the UF Health Shands Core Laboratory is on the road to becoming fully automated, providing staff with more advanced technology and additional workspaces.
We also began a long-term collaboration between UF Health Shands Rehab Hospital and Select Medical to build on our already outstanding rehab care and take programs there to the next level. We plan to use Select Medical’s academic health center model, used at centers such as the well-respected Kessler Institute for Rehabilitation. We have an interim management agreement underway with plans for shared ownership and Select Medical’s oversight for rehab hospital operations. Our relationship with Select Medical also includes co-ownership of the Select Specialty Hospital – Gainesville on Archer Road. Our College of Medicine physicians will join the medical staff and focus on quality care and patient safety.
Our strength as a regional health care resource continues to grow as we care for more patients from throughout Florida. In 2016, UF Health Shands treated patients from all 67 counties in Florida, affirming our reputation as the state’s primary hospital. We’ve broadened our presence in Pensacola with the Sacred Heart Health System collaboration and continue to explore other opportunities to help improve care and meet the needs of patients throughout the region and state. Just this month, UF Health Physicians debuted two new practices in Marion County — UF Health Ocala Health Brook and UF Health Villages. Both practices serve cardiology patients, and orthopaedic services also will be offered at UF Health Villages in the spring. And in the fall, when Hurricane Matthew hit, UF Health Shands fulfilled our role as a first-receiver in regional emergencies. We were trusted to treat patients evacuated from other hospitals and were on standby for mass casualties and to support our colleagues in Jacksonville.
I hope you join me in feeling great pride for all we’ve accomplished together this past year. It’s an honor to be part of the UF Health family and work with such talented and caring colleagues. Every day, I hear stories about how all of our hospital teams collaborate to heal and support patients and their loved ones, providing care that goes beyond their physical and medical needs to include their emotional and social needs.
A great example comes to mind. Recently, our UF Health Shands Hospital Intermediate Care Unit 94 staff cared for a young mother. Her medical condition and quickly declining health meant she would not be home to celebrate her son’s birthday, which was a few days away. The unit mobilized for this family. They found out the little boy loved Power Rangers and threw him a themed birthday party in her room that the family could enjoy together. Our nursing staff went all out with decorations, a cake and gifts. The medical team stopped by to help make it festive. During the party, the boy curled up in his mom’s lap, spending some final moments with her. Someone captured that special moment with a photograph. Sadly, the mom has since passed away. Weeks later, a family member visited the unit to share something meaningful with our team: The photograph of the mother and her son curled up is now in a custom frame that the nursing team made for them. The team learned that the boy keeps the frame by his bed and uses it to kiss his mom goodnight.
I hear stories like this all the time and they fill me with admiration for the investment you make to care for others. Every kindness and extra effort you offer can make an immeasurable impact on our patients and their loved ones. You are making a huge difference every day, in small as well as dramatic ways. So for everything you do, I thank you. I can’t wait to see what we accomplish in 2017. Go Gators!
UF Health Jacksonville
CEO: Russell E. Armistead, M.B.A.
 2016 was an exceptional year for UF Health Jacksonville. The organization exceeded its economic objectives and made significant progress in quality improvement. We were especially pleased to achieve a three-star ranking with Vizient. As with any goal, now that we have achieved this, we have our sights set on a four-star rating!
2016 was an exceptional year for UF Health Jacksonville. The organization exceeded its economic objectives and made significant progress in quality improvement. We were especially pleased to achieve a three-star ranking with Vizient. As with any goal, now that we have achieved this, we have our sights set on a four-star rating!
In September, UF announced the appointment of Leon L. Haley Jr., M.D., MHSA, FACEP, C.P.E., as the dean for the University of Florida College of Medicine – Jacksonville. He officially started his new role on Jan. 4, 2017. Dr. Haley came to UF Health from Atlanta, where he was a professor of emergency medicine and executive associate dean for the Emory University School of Medicine and a key administrator at Grady Memorial Hospital, the city’s safety-net hospital. Dr. Haley received his medical degree from the University of Pittsburgh and a master’s degree in health services administration from the University of Michigan. He is board-certified in emergency medicine and is a Fellow of the American College of Emergency Physicians.
This year allowed us to make significant inroads in community support. The success of our Night for Heroes and RITA golf events allowed more local decision makers to learn about what we do and the positive impact we make on the community. In addition, the Jacksonville Civic Council continues to work with us to explore ways to enhance funding to care for the city’s uninsured population.
As you will see below, the UF Health Jacksonville team produced numerous accolades and real results. I continue to be proud of these efforts, each focused on bringing real benefits to our community and to each patient we serve.
Quality
Vizient Three-Star Rating: Devotion to patient care is one reason why UF Health Jacksonville went from a two-star to a three-star rating in the 2016 Vizient Quality and Accountability Score. Vizient evaluates more than 100 academic health centers and measures their patient outcomes, patient safety and mortality rates. We showed consistent improvement in many specific measures. This means our patients are not only experiencing fewer complications, but are also less likely to be readmitted.
 Innovation Award: In the fall, Vizient honored UF Health Jacksonville with its inaugural Innovation Excellence Award. This accolade recognized the hospital for developing an innovative technology solution that has enhanced our patient care delivery models. A group of UF Health Jacksonville staff launched the Sepsis Program Protocol in 2014. The program runs in the background of EPIC and sends alerts to physicians and nurses about patients who are at risk of developing sepsis. The software has helped us drop our sepsis rate by 30 percent, and was noted as a model for other health care organizations.
Innovation Award: In the fall, Vizient honored UF Health Jacksonville with its inaugural Innovation Excellence Award. This accolade recognized the hospital for developing an innovative technology solution that has enhanced our patient care delivery models. A group of UF Health Jacksonville staff launched the Sepsis Program Protocol in 2014. The program runs in the background of EPIC and sends alerts to physicians and nurses about patients who are at risk of developing sepsis. The software has helped us drop our sepsis rate by 30 percent, and was noted as a model for other health care organizations.
Magnet Redesignation Last summer, the American Nurses Credentialing Center renewed UF Health Jacksonville’s status as a Magnet® organization, once again singling out the hospital and staff for the excellent work done here each day. It is the highest designation for nursing excellence and an honor bestowed on less than 8 percent of hospitals in the United States.
Chest Pain Center The Society of Cardiovascular Patient Care recognized UF Health Jacksonville’s proactive cardiac treatment as one of the best in the country and awarded the Chest Pain Center with Primary PCI and Resuscitation Accreditation. UF Health Jacksonville’s Chest Pain Center is one of only 24 health care facilities — and the only one in Florida — to receive this accreditation. Chest pain centers with primary PCI (percutaneous coronary intervention) and resuscitation are considered the most prepared among health care facilities. The two-year-long accreditation process is one of the most rigorous reviews in our industry. It brings together diverse medical specialties, including emergency medicine, cardiology, neurology and internal medicine.
Improvements in Hospital-Acquired Conditions UF Health Jacksonville formed a task force composed of hospital administrators, surgeons, nurses and others to analyze processes and procedures in surgery. The group started by using the capabilities EPIC already has in place. The software helps with early recognition of infections by monitoring vital signs and sending alerts when there are factors present that indicate sepsis. In addition, staff created the Sepsis Program Protocol to pull vital signs and lab values every hour for each patient in the hospital. The team is currently working toward integrating a recognition tool into EPIC and possibly including a risk calculator.
Additionally, over the past year, surgical clinics used the antiseptic chlorhexidine gluconate, or CHG, to reduce surgical site infections. Since the initiative began, postsurgical sepsis infections dropped from 4.7 percent in 2015 to 1.62 percent in 2016.
Organ Procurement UF Health Jacksonville holds an annual ceremony honoring patients who gave the gift of life through organ donation. Our Donor Council is responsible for the many recognitions around the hospital that honor organ donors: a purple butterfly placed outside the door of the operating room, a purple blanket is placed on the patient during his or her final moments, and the Donate Life flag is flown outside the Clinical Center for three days after the patient’s passing. In addition to these efforts, the Donor Council is responsible for the Tree of Life in the East Expansion of the Clinical Center, where leaves represent adult patients and butterflies represent pediatric patients. Twenty-one patients gave the gift of life, donating 80 organs in 2016.
People
More Than Half a Century of Service Employee satisfaction and loyalty are evidenced by the lengthy tenure of many of our staff members. Milestone anniversaries are celebrated at an awards ceremony every year during Hospital Week. In 2016, a very special anniversary was recognized as Cecil Wright marked her 55th year with UF Health Jacksonville.
New B.S.N. Programs A collaboration with the UF College of Nursing three years ago resulted in the establishment of an accelerated course of study for students with a bachelor’s degree or higher in another field who wish to pursue a bachelor’s in nursing. The accelerated B.S.N. program builds on previous learning experiences and transitions individuals with undergraduate and graduate degrees in other fields into nursing. The program is 16 months long and consists of four consecutive semesters of full-time study. In addition, UF now offers an R.N.-to-B.S.N. online program.
Satisfaction and Recognition Retaining good employees is an essential key to our success, which is why we place great emphasis on employee satisfaction. Every summer, we conduct our employee engagement survey. Our results improved from the 43rd percentile in 2015 to the 76th percentile in 2016! We also ranked above the national average in many areas, including:
- Overall employee satisfaction
- Confidence in management’s leadership
- Fairness of pay compared with other health care employers in this area
- Feeling of belonging to the organization
- Sufficient time to provide best care and service to clients and patients
Last year, we received the First Coast Worksite Wellness Council’s Platinum Award and the American Heart Association’s Fit Friendly Organization Gold Award. The Jacksonville Business Journal recognized four of our faculty and staff as Health Care Heroes: Chad McIntyre; Rita Nathawad, M.D.; Barry Steinberg, M.D., D.D.S.; and David Vukich, M.D.
Hurricane Matthew While other hospitals in Jacksonville and surrounding communities evacuated patients and even closed due to their locations or capabilities, we did not. UF Health Jacksonville and UF Health North remained open throughout the storm. Hundreds of employees lived and worked on our campuses from Thursday through Saturday. Our physicians, nurses, other patient caregivers and support staff worked tirelessly to ensure our patients and guests continued to receive the best care possible.
Service
Hospitality More than 7,500 UF Health physicians, residents, staff and contract vendors at UF Health Jacksonville, UF Health North and our practices throughout Northeast Florida and Southeast Georgia completed Hospitality Standards of Behavior training.
Last year, we redesigned our Applause recognition program to incorporate the UF Health Hospitality Standards to support our efforts to recognize employees for demonstrating their commitment to improving the patient experience as well as our interactions with one another.
Growth
Oncology Services Our outpatient oncology services expanded with the opening of three additional oncology infusion centers in Orange Park, Fernandina Beach and North Jacksonville (at UF Health North). These new centers signaled the completion of our oncology program expansion that began in 2015 with the opening of centers in Baymeadows on Jacksonville’s south side and LaVilla in downtown Jacksonville.
UF Health North
Opened in February 2015, UF Health North continues to exceed expectations, with the Emergency Department in the 95th percentile for overall quality of care and Outpatient Surgery in the 90th percentile for overall quality of care, according to PRC patient satisfaction scores.
Celebrations We honored former Methodist Medical Center CEO and one of Northeast Florida’s longtime leaders in the medical community with the naming of the Marcus E. Drewa Atrium on Feb. 25. A month later, we hosted a community health fair to celebrate the one-year anniversary of the medical office complex opening. And in May, we held a beam-raising ceremony to mark the installation of the final beam in the bed tower expansion.

Continued Growth Last year, we:
- Opened a dedicated blood-drawing suite in October.
- Successfully opened UF Health Oncology – North in January.
- Opened dedicated suites for UF Health Women’s Specialists, UF Health Occupational Medicine and UF Health Orthopaedic Surgery in August.
- Opened the dedicated suite for UF Health Neurosciences in December.
Phase II: Bed Tower Despite a somewhat busy hurricane season, construction of our 92-bed community hospital remains on budget and ahead of schedule, and we expect to open in late spring. The five-story all-private patient room hospital will include a 12-bed labor and delivery and postpartum unit, two cesarean operating rooms and an eight-bed women’s services unit on the second floor. The third floor will house a 24-bed intensive care unit. There will 24 medical/surgical suites on the fourth floor and an additional 24 on the fifth floor.


Finances In addition to our financial improvement, achieving a positive margin of $20.6 million for the fiscal year ending June 30, 2016, we maintained our investment grade ratings from both Moody’s and Fitch rating agencies, after borrowing an additional $85 million for construction of the 92-bed tower in the North.
UF Health North has generated a steady stream of admissions from the ER to the main campus downtown, with an average of 13 patients admitted per day, resulting in 46 inpatients from the north campus on any typical day.
Concluding remarks: The breadth and depth of the achievements of faculty and staff at our academic health center, as summarized in this “Year in Review,” is always humbling and inspiring. It doesn’t get old! And the trajectory of our success has not reached a plateau! Indeed, building on the amazing progress highlighted across all of our colleges, research institutes and hospitals, I am confident that the best is yet to come. I wish you all the very best for 2017 and look forward to working with you to achieve our goals.
Power of Together,
David S. Guzick, M.D., Ph.D. Senior Vice President for Health Affairs, UF President, UF Health
About the author
