UF clinical trial tests efficacy of drug to treat a rare, and often deadly childhood disease
A University of Florida researcher with a $2 million federal grant is launching the first Phase III clinical trial for treatment of a congenital disease of the mitochondria, the energy powerhouse of cells.
A Phase III trial assesses a treatment’s efficacy in patients and is one of the last steps necessary before Food & Drug Administration approval.
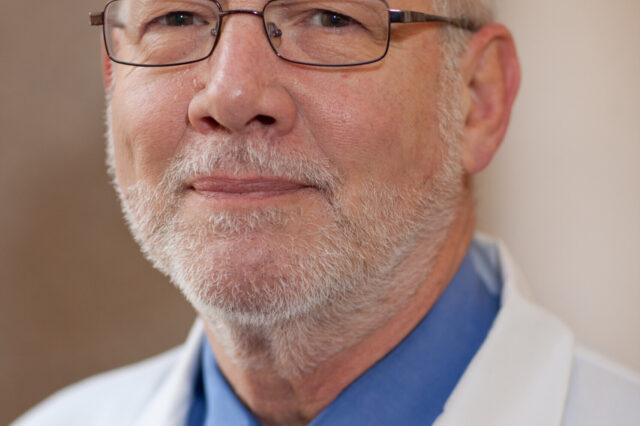
The trial, conducted by Peter W. Stacpoole, M.D., Ph.D., a professor of medicine, biochemistry and molecular biology, will assess a new drug therapy for one of the rarest childhood diseases, pyruvate dehydrogenase complex deficiency, or PDC.
The disease, caused by a genetic mutation, afflicts 200 to 300 children in the United States at any one time. By interfering with the cell’s ability to produce energy, it can leave them profoundly disabled, with severe neurological and neuromuscular degeneration.
There are currently no FDA-approved treatments for PDC, and many patients do not survive childhood.
Funded by a $2 million grant from the FDA, Stacpoole is assessing the effectiveness of a drug treatment developed from a molecule called dichloroacetate, or DCA, which is similar to the vinegar molecule. “I often call it vinegar with a kick,” Stacpoole said.
Stacpoole has researched dichloroacetate most of his career, publishing his first paper involving the molecule in 1969 as a graduate student.
PDC interferes with the chemical reactions in the cell necessary to produce energy. But Stacpoole said DCA stimulates residual activity in a critical enzyme — enzymes accelerate chemical reactions — allowing the cell to produce additional energy.
The drug is not considered a cure for PDC, but this study may finally determine if DCA is effective and thus may mitigate the effects of the disorder and provide hope to parents with no other treatment options, Stacpoole said.
He noted that the clinical trial will demonstrate whether “these children’s functionality, their ability to improve their quality and even possibly their quantity of life, may be enhanced by stimulating this enzyme that is so critical to energy metabolism.”
The trial involves 30 children from across the country, who will at different times receive either dichloroacetate or a placebo. All will receive dichloroacetate at some point on a rotating basis, Stacpoole said.
Parents will be asked to complete a daily survey during the nine-month trial describing how their children are doing, he said. Things the parents will be asked to observe and rate on a scale are changes in muscular strength, seizure activity, and stomach or gastrointestinal problems.
“We think this drug is very safe for children,” Stacpoole said. “However, DCA can cause reversible peripheral nerve damage that has mainly been seen in adults, who metabolize the drug more slowly than children. But we’ll be looking for this potential adverse effect in the trial. Regardless, a Phase III clinical trial is really the ultimate test of the chronic safety and efficacy of any kind of investigational drug, whether it’s for a rare or common disease.”
Stacpoole said it has been a challenge through the years attracting pharmaceutical funding for research on PDC, a common difficulty with rare diseases. Drugs to treat such rare disorders are commonly called orphan drugs.
“So, the development of DCA has been slow and dependent on our ability to receive federal funding every step of the way,” he said.
The latest FDA grant was awarded in 2016 and is funded by an agency grant program to fund orphan products clinical trials. The program has provided more than $370 million to fund at least 590 clinical studies since its creation in 1983.
About the author
