Progress in NIH Funding at UF Health
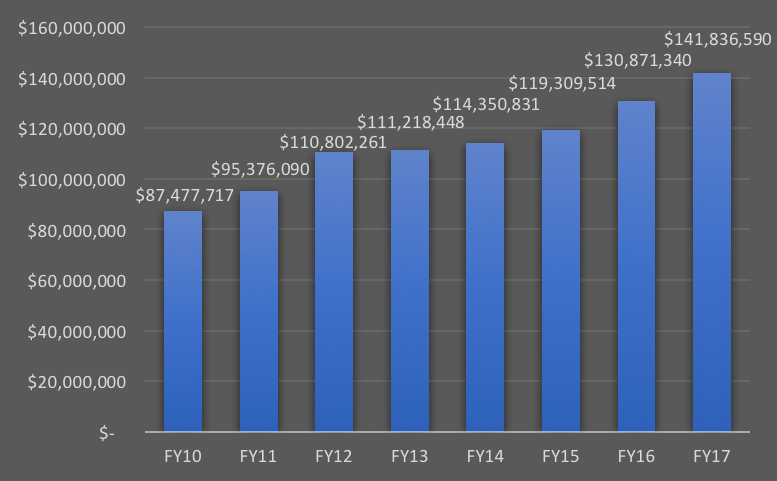
The fiscal year for the National Institutes of Health ended on Sept. 30, and I have good news to report: NIH funding at UF Health, the university’s academic health center, is up for the seventh consecutive year and now totals $141.8 million, based on preliminary (but solid) estimates.
Of course, there are many ways to measure success in academic health science research, such as quantity and quality of publications, scientific impact of translational studies, and patents and licensing agreements. The metric most commonly used by most ranking systems, however, and by individuals in leadership positions at peer institutions, is total grant awards from NIH in which faculty were Principal Investigators.
In our Forward Together Strategic Plan, published on May 20, 2010, our motto for research was “reach for excellence,” and a number of strategies were identified and subsequently implemented in our quest for research stature. Momentum in research commenced and accelerated over the next five years, with fortuitous timing regarding the state-funded UF preeminence initiative, which coincided with the planning of our Power of Together Strategic Plan, published on May 20, 2015.
Due to the talent, dedication and persistence of faculty and staff across UF Health, there has been consistent improvement in NIH funding, despite the essentially flat NIH national budget that has created an extremely challenging funding environment. There is no higher compliment that can be paid to an academic biomedical researcher in the United States than to garner the enthusiastic support of scientific peers at an NIH Study Section sufficient to warrant a fundable grant score. This recognition of the scientific excellence of the research conducted by UF faculty at UF Health has translated into the trajectory shown in the graph below. I am grateful to Dr. Steve Sugrue for assembling these data; the figures for 2017 are preliminary:
While the ability of each college to participate in research has varied, each has contributed to the overall increase:
|
Medicine |
Dentistry |
Nursing |
Pharmacy |
Public Health & Health Professions |
Veterinary Medicine |
|
| FY10 |
$62,058,946 |
$9,499,790 |
$91,942 |
$5,794,077 |
$7,674,505 |
$2,358,457 |
| FY11 |
$72,157,623 |
$7,862,530 |
$92,089 |
$5,896,358 |
$8,120,292 |
$1,247,198 |
| FY12 |
$83,890,252 |
$7,621,368 |
$5,085,993 |
$11,596,841 |
$2,607,807 |
|
| FY13 |
$84,898,636 |
$7,311,139 |
$828,944 |
$5,431,498 |
$9,701,648 |
$3,046,583 |
| FY14 |
$88,002,897 |
$8,675,501 |
$418,767 |
$5,060,700 |
$9,035,677 |
$3,157,289 |
| FY15 |
$89,517,847 |
$7,747,001 |
$412,236 |
$5,083,640 |
$11,183,473 |
$5,365,317 |
| FY16 |
$93,638,074 |
$9,750,508 |
$1,049,998 |
$6,315,314 |
$13,664,071 |
$6,453,375 |
| FY17 |
$101,609,557 |
$9,479,563 |
$783,101 |
$6,674,804 |
$14,409,329 |
$8,880,236 |
Of special note is the College of Medicine, which this year eclipsed $100 million in funding; the colleges of Nursing, Pharmacy, Public Health and Health Professions, and Veterinary Medicine, all of which have shown a significant upward trajectory recently; and the College of Dentistry, which has maintained its top 10 ranking among U.S. dental schools over the entire period (currently ranked No. 7).
To provide readers a flavor of the richness and breadth of our faculty science funded by NIH, here is a cross-section of some of the larger grants we have recently been awarded:
 Donald C. Bolser, Ph.D., Professor, Department of Physiological Sciences
“Functional mapping of peripheral and central circuits for airway protection and Breathing” and “Modeling the role of NTS in the neurogenesis of airway defensive behaviors”
Donald C. Bolser, Ph.D., Professor, Department of Physiological Sciences
“Functional mapping of peripheral and central circuits for airway protection and Breathing” and “Modeling the role of NTS in the neurogenesis of airway defensive behaviors”
Dr. Donald Bolser is the PI of a three-year, $7.5 million grant from the NIH titled “Functional mapping of peripheral and central circuits for airway protection and breathing.” This award will fund research to map peripheral and central nervous systems pathways that control respiratory muscles. The NIH program that has funded this grant is known as SPARC (Stimulating Peripheral Activity to Relieve Conditions) and is a six-year program aimed at increasing our knowledge of major organ systems so that new neuromodulatory devices can be developed for treatment of visceral disease processes. A major emphasis of the project is how the parts of the nervous system that control lung function adapt and change in response internal and external events, a process known as neuroplasticity. They also are investigating how the nervous system is organized to produce behaviors that allow us to protect our airways, such as coughing. The loss of effective coughing is linked to a high rate of pneumonias in patients with neurological diseases such as Parkinson’s disease, spinal injury, traumatic brain injury and Alzheimer’s disease.
The grant builds on the collective work of existing faculty here at UF who have specific skill sets in the control of breathing. An important feature facilitating how this team functions is the Center for Respiratory Research and Rehabilitation, headed by Dr. Gordon Mitchell, which brings together faculty members who focus on respiratory research from all over the Gainesville campus. Faculty from three health colleges — the College of Veterinary Medicine, the College of Medicine and the College of Public Health and Health Professions — have important roles in the project. Furthermore, the grant represents a partnership with the Morsani College of Medicine at the University of South Florida as well as the Kentucky Spinal Cord Research Institute at the University of Louisville.
Dr. Bolser is also the PI of a four-year, $3 million grant from NIH titled “Modeling the role of the NTS in the neurogenesis of airway defensive behaviors.” This award will fund research into how neural networks in the brain protect our airways from aspiration by activating coughing. A major emphasis of this research is the neural mechanisms that are responsible for the actions of cough suppressant drugs.
 Robert L. Cook, M.D., M.P.H., Professor of Epidemiology and Medicine, and Associate Director of the Florida Center for Medicaid and the Uninsured
Health Outcomes and Cognitive Effects of Marijuana Use in Persons Living with HIV/AIDS
Robert L. Cook, M.D., M.P.H., Professor of Epidemiology and Medicine, and Associate Director of the Florida Center for Medicaid and the Uninsured
Health Outcomes and Cognitive Effects of Marijuana Use in Persons Living with HIV/AIDS
In January, Florida’s Amendment 2 took effect, granting citizens with serious illnesses, including HIV, legal access to medical marijuana. While there is some evidence that marijuana may improve HIV-related symptoms, there is still a lot experts do not know about its health effects. University of Florida researchers hope to answer some of these questions with a new study supported by a $3.2 million R01 research grant from the National Institute on Drug Abuse. During the five-year study, UF researchers and partners at the University of South Florida and Florida International University plan to follow 400 Floridians with HIV who report current marijuana use. It is believed to be the largest and most comprehensive study to date on the health effects of marijuana in people with HIV. The research team will track the quantity, frequency and cannabinoid content of marijuana used by participants in order to identify the patterns of use most strongly associated with control of patient symptoms, such as pain, stress and sleep problems. The team will evaluate marijuana’s effect on participants’ health outcomes, such as HIV viral suppression and biological markers of chronic inflammation, and through neurocognitive testing, they hope to gain an understanding of how marijuana may affect thinking, memory and planning in people with HIV. The researchers will also compare health outcomes and potential consequences in people who receive medical marijuana with outcomes and consequences in those who use recreationally. The research team includes scientists from several different disciplines, and includes expertise from public health, clinical medicine and basic science.
 Susan Nittrouer, Ph.D., Professor and Chair, Department of Speech, Language, and Hearing Sciences
Spoken Language in Adolescents with Hearing Loss
Susan Nittrouer, Ph.D., Professor and Chair, Department of Speech, Language, and Hearing Sciences
Spoken Language in Adolescents with Hearing Loss
Childhood hearing loss has traditionally imposed severe constraints on language and literacy development, but at the end of the last century hope was born that these constraints might be mitigated by the advent of two technologies: methods for identifying hearing loss shortly after birth and a device for bypassing damaged inner-ear structures to stimulate the auditory nerve directly. The goal of this project is to see how well that hope is being realized. It is a continuation of a longitudinal study involving 124 children with and without hearing loss from across the country. These children are now adolescents, just completing middle school. They will visit the University of Florida across three summers to be tested on a variety of skills, including complex auditory processes, speech perception, language abilities and reading. When combined with data from these children going back as far as infancy, we will be able to construct growth models specifying how various factors influenced the language, cognitive and social development of these children. Outcomes should inform future design of clinical and educational programs for children with hearing loss.
 Marco Pahor, M.D., Professor and Founding Chair, Department of Aging and Geriatric Research, and Director, Institute on Aging
UF Claude D. Pepper Older Americans Independence Center
Marco Pahor, M.D., Professor and Founding Chair, Department of Aging and Geriatric Research, and Director, Institute on Aging
UF Claude D. Pepper Older Americans Independence Center
The mission of the UF Claude D. Pepper Older Americans Independence Center is twofold: 1) to optimize older persons’ physical performance and mobility through interdisciplinary approaches; and 2) to train new investigators in aging and disability research while developing their leadership qualities. Our goal is to enhance late-life health and independence, with a special focus on mobility. To accomplish our mission, our strategy is to attract studies and inventive investigators from diverse behavioral, clinical, basic and technological science disciplines with a common research focus: “mobility and prevention of disability.” Traversing the entire spectrum of biomedical investigation, including molecular biology, animal studies, clinical research, behavioral sciences, epidemiology and engineering, our research effort addresses the Pepper OAIC’s general goal: to increase scientific knowledge that leads to better ways to maintain or restore independence of older people. During the past five years, the UF Pepper OAIC has supported over 80 investigators, mentors, Junior Scholars and affiliated scholars across multiple colleges and departments. The Pepper OAIC pilots have provided preliminary data for developing several large multicenter NIH trials, including LIFE, ENRGISE, ACT, TTrials and MOTRPAC. Its total impact on UF aging-related grants has been 125 grants, 40 of which are from Junior Scholars, with a total cost of over $207.6 million. The UF Pepper OAIC has just been awarded its third five-year competitive renewal, a testimony of its success.
 Rolf Renne, Ph.D., Professor, Department of Molecular Genetics and Microbiology, and Associate Director for Basic Sciences, UF Health Cancer Center
Non-coding RNAs in Gamma-herpesvirus biology and AIDS malignancies
Rolf Renne, Ph.D., Professor, Department of Molecular Genetics and Microbiology, and Associate Director for Basic Sciences, UF Health Cancer Center
Non-coding RNAs in Gamma-herpesvirus biology and AIDS malignancies
In February, a team led by Dr. Rolf Renne, Ph.D., a professor of molecular genetics and microbiology at UF, received an NCI Program Project titled “Noncoding RNAs in Gamma-Herpesvirus Biology and AIDS Malignancies.” The program includes three projects, two at UF and one at Tulane University in New Orleans. Dr. Renne, who serves as associate director of basic sciences for the UF Health Cancer Center, studies the biology and pathogenesis of Kaposi’s sarcoma-associated herpesvirus, or KSHV, a human pathogen associated with skin cancer and B cell lymphomas in AIDS patients. Dr. Scott Tibbetts, also from molecular genetics and microbiology, studies a related mouse virus, Murine herpesvirus 68 (MHV68), a model system for γ-herpesvirus cancers. A third project, led by Dr. Erik Flemington, of Tulane University, studies Epstein-Barr virus, or EBV, a second cancer-causing human herpesvirus. The project creates synergy between all three laboratories, and will explore pathways regulated by long non-coding RNAs (lncRNAs) that contribute to γ-herpesvirus tumors. The project is supported by two service cores: a Bioinformatics and RNA sequencing core at Tulane University directed by Dr. Flemington, and a Viral Genetics core at UF led by Dr. Renne. Additional UF support enables these cores to provide annual hands-on training workshops to UF and Tulane program staff. The project is supported by a clinic at LSU that treats AIDS patients who suffer from KSHV- and EBV-associated malignancies and will provide clinical specimens. This program project, the first such multi-investigator grant at the UF Health Cancer Center, will receive a total of $1.3 million per year over five years.
 Desmond Schatz, M.D., Professor and Associate Chair, Department of Pediatrics, and Medical Director, UF Diabetes Institute
Non-invasive detection of cell death in type 1 diabetes
Desmond Schatz, M.D., Professor and Associate Chair, Department of Pediatrics, and Medical Director, UF Diabetes Institute
Non-invasive detection of cell death in type 1 diabetes
The University of Florida’s Type 1 diabetes program is internationally recognized. Led by Drs. Desmond Schatz and Mark Atkinson, the program has outstanding collaborations nationally and internationally. The project is a collaboration between Schatz (University of Florida), Yuval Dor (Hebrew University, Jerusalem, Israel) and Carla Greenbaum (Benaroya Research Institute, Seattle). The investigators have a long history of joint efforts in Type 1 diabetes and are actively involved in multiple NIH-funded studies collaborative studies, including TrialNet, ITN, TEDDY and nPOD, among others.
Detection of beta cell damage or death in blood is an important challenge that could transform basic research, diagnosis and clinical trials in diabetes. Dr. Schatz and his collaborators have so far identified dozens of DNA methylation markers unique to β cells and additional cell types, and developed a method to detect these markers in plasma, resulting in high sensitivity and specificity in the detection of death of β cells and other cell types. Herein, and building on a history of collaboration, studies in this grant seek to optimize and validate this sensitive qualitative assay, to allow the simultaneous detection of multiple methylation markers for sensitive identification of cell death in multiple tissues in Type 1 diabetes. The overall goal is to determine altered turnover of β cells, pancreatic exocrine cells and T cells, prior to and during the development of Type 1 diabetes and ultimately perform a methylome-wide analysis of Type 1 diabetes plasma. Such data will facilitate a better understanding of cell death in Type 1 diabetes, and enable the development of markers to assess interventional strategies.
 Lee Sweeney, Ph.D., Professor, Department of Pharmacology and Therapeutics, and Director, UF Myology Institute
UF Wellstone Muscular Dystrophy Cooperative Center
Lee Sweeney, Ph.D., Professor, Department of Pharmacology and Therapeutics, and Director, UF Myology Institute
UF Wellstone Muscular Dystrophy Cooperative Center
Dr. Lee Sweeney received a grant from NIH (NIAMS) titled, “Failed Regeneration in the Muscular Dystrophies: Inflammation, Fibrosis and Fat.” This grant funds one of six Wellstone Muscular Dystrophy Cooperative Centers in the U.S. These centers were established by an act of Congress (MD Care Act). The goals of the UF Wellstone Center are to identify the causes of muscle replacement in animal models of Duchenne muscular dystrophy, evaluate potential therapeutics to allow more successful regeneration, and develop imaging techniques to examine the impact of the therapies on patients. Dr. Sweeney is joined in the center efforts by Drs. Glenn Walter (College of Medicine) and Krista Vandenborne (Public Health and Health Professions), who jointly focus on development of MR imaging of muscle disease; Dr. Elisabeth Barton (Health and Human Performance), who focuses on evaluating animal models of disease; and Dr. Andy Judge (Public Health and Health Professions), who directs the center’s training efforts. The center also has participating investigators at UCLA and Northwestern University.
The Power of Together,
David S. Guzick, M.D., Ph.D. Senior Vice President for Health Affairs, UF President, UF Health
About the author
