Separation of Conjoined Twins
When Jacquelyn was 20 weeks pregnant, she and her partner, Mark, visited her obstetrician to have an ultrasound to find out the sex of their baby. Up to that point, they thought that Jacquelyn was carrying only one, since earlier sonograms captured only one heartbeat. The ultrasound revealed there were two babies, however, and the reason for the one heartbeat was that they were conjoined at the heart, beating in synch. The twins were also conjoined at the liver, diaphragm and sternum.
Needless to say, this was quite a shock. The news for Jacquelyn and Mark was also very sad, since they were told that the twins would likely be delivered stillborn, or, if born alive, would probably not survive more than a few days after birth. Indeed, about 40 to 60 percent of conjoined twins are delivered stillborn, and about 35 percent survive only one day. Surgery can be performed to separate conjoined twins, but survival in the case of conjoined hearts is extremely rare.
Jacquelyn and Mark sought other opinions, and ultimately visited Jennifer Co-Vu, M.D., an assistant professor of pediatrics. Dr. Co-Vu is a pediatric cardiologist who directs the fetal cardiac program at UF Health. Dr. Co-Vu studied the anatomy of the conjoined twins during an hourlong session of imaging studies, and in particular the anatomy of the two hearts and how they were connected. She concluded that with appropriate medical care, the twins could survive for a period of time after birth, and that there may be a way to separate the hearts surgically in a manner that would allow long-term survival. After finding out as much as they could about their options, and carefully considering the risks and benefits of surgery, Jacquelyn and Mark decided to proceed along a path that would lead to surgical separation of the twins after birth.
The team at the UF Health Congenital Heart Center sprung into action. In addition to Dr. Co-Vu, the team included:
- Mark Bleiweis, M.D., the William G. Lassiter Jr. and Aneice R. Lassiter professor of surgery and pediatrics, chief of pediatric cardiovascular surgery and director of the UF Health Congenital Heart Center;
- Saleem Islam, M.D., M.P.H., professor of surgery and pediatrics and chief of pediatric surgery;
- Monique Ho, MD, assistant professor of obstetrics and gynecology in the division of maternal-fetal medicine;
- Sandra Sullivan, MD, associate professor of pediatrics in the division of neonatology;
- Ashley Lentz, M.D., assistant professor of surgery in the division of plastic surgery; and many other faculty and staff from these units, along with
- Dhanashree Rajderkar, M.D., assistant professor and chief of pediatric radiology; and
- Andrew Pitkin, MBBS, associate professor of anesthesiology and medicine.
Many other faculty and staff from these and other units also contributed significantly.
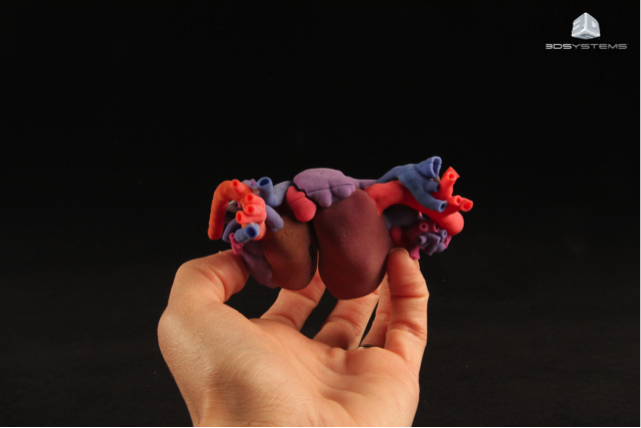
Dr. Co-Vu submitted cardiac and liver images from CT and MRI scans to 3D Systems, a company from Colorado that prints 3-D models. A 3-D true-to-size model of the twins’ conjoined hearts was created, which appears to be the first 3-D printed conjoined heart. This replica, shown below, allowed Dr. Co-Vu and Dr. Bleiweis to create proactively a plan for the cardiac portion of the surgery that was based on the specific anatomy of the twins’ hearts.
After hundreds of hours of meetings of all the faculty and staff involved, a detailed plan evolved for prenatal care, delivery, neonatal care, the actual surgery (sternum, heart, diaphragm, liver) required to separate the twins, and a series of surgical procedures needed to address additional congenital problems as well as to close the large defects in the chest and abdominal walls of the two babies. Needless to say, despite a plan with enormous detail, some revisions were needed as events unfolded, depending on clinical circumstances.
After careful prenatal care by the maternal-fetal medicine team, Scarlett and Savannah were born in April 2016 at 35 5/7 weeks gestation via C-section at the UF Health Shands obstetrical unit. They were transferred to the neonatal intensive care unit, where the physiology of their conjoined hearts, diaphragms and a single large liver was managed in a way that allowed them to develop sufficiently to allow surgical separation. This occurred in June. Since then, Scarlett and Savannah have undergone a total of 10 additional surgical procedures and have spent several months in the pediatric intensive care unit. While they will need to meet many more challenges ahead, these two baby girls are clearly strong and up to the challenge. They can be seen in their “twin stroller” below.

Identical twins occur when a single fertilized egg divides to create two identical embryos, which develop into two identical fetuses. In the case of conjoined identical twins, which occur in about 1 in 200,000 births, the embryo division process is incomplete, resulting in connections between the twins at the level of one or more organ systems. Only about 250 successful surgical separations have been accomplished in which one or both twins have survived long term; of these, until now there have been extremely few successful separations in cases of a conjoined heart.
It is illuminating and inspiring to hear from some of the faculty and staff who have been involved in the care of Jacquelyn, Scarlett and Savannah.
Dr. Jennifer Co-Vu: “We are extremely fortunate to have such a great team at UF Health Shands Children’s Hospital — from the fetal sonographers, nurses, OR staff, radiology staff, ICU, fellows, residents and subspecialists — it was heartwarming to have been given the opportunity to give Scarlett and Savannah a chance to live a normal, separated, life.”
Dr. Mark Bleiweis: “Separating and caring for Savannah and Scarlet — with the daunting situation of a conjoined heart — required seamless planning, execution, teamwork and communication. Because of outstanding preoperative, intraoperative and postop care, Mark and Jacquelyn can see a future for their beautiful baby girls. I feel so blessed to be part of a UF Health team that can handle the most complex situations with superb skill and grace.”
Dr. Saleem Islam: “This was an extremely complex, high-risk undertaking — and it took a village of highly skilled and trained individuals to pull it off. The liver anatomy was unique in that there was no plane of separation and we had to create one intraoperatively, assuring that both babies had enough to survive. After the separation procedure the babies both needed multiple operations to gradually reconstruct the diaphragm and close the defect with biologic mesh. We are certainly grateful that the babies did so well.”
Dr. Andrew Pitkin (anesthesiologist): “It is difficult to describe adequately the complexity of managing two small infants undergoing major surgery in an operating room that has been designed for one patient at a time. The success of this procedure shows that an experienced and cohesive team can overcome every size of obstacle, from preventing confusion between the babies’ lines (orange and blue tape) to dealing with complex and uniquely abnormal cardiac physiology.”
Dr. Sandra Sullivan: "The teamwork in action at the girls' delivery was incredible. Dr. Collins, pediatric ENT, stood by all morning with his team in an adjacent operating room, to support my neo resuscitation team. Ultimately, the girls were born and breathed spontaneously. It was my privilege to "catch" the girls, be one of the first people to meet them, and take care of these little miracles for the subsequent weeks."
Dr. Monique Ho: “This is one example of the superlative combination of communication, thoughtful planning and situational agility that this committed multidisciplinary team exhibits every single day. Our goal is always to bring families through one of the most difficult times in their lives in the least stressful way possible; one that is specifically individualized to their unique needs and achieves the best of the potential outcomes. I always find it rewarding to be part of this process.”
From a hospital perspective, UF Health Shands CEO Ed Jimenez states: “Dozens of experts at UF Health collaborated to painstakingly plan and perform incredibly complex procedures to help the twins. Their remarkable expertise resulted in an extraordinary milestone to help the babies and their loving family. Our UF Health teams have amazing capabilities and strive to provide the best possible outcomes for every patient. This determination has led to fantastic results. Our overall hospital survival rate for pediatric cardiac surgery is 98.7%.”
That Jacquelyn and Mark will be able to take home Scarlett and Savannah as two independent identical twin children is the kind of outcome to which all we all aspire at UF Health. It represents the work of not only a group of faculty and staff who are uniquely capable in the technical aspects of the diagnosis and treatment of the rare and life-threatening condition that befell Scarlett and Savannah at birth, but equally important, an unparalleled level of commitment and teamwork in pulling off this miracle. We all wish this special family the very best for the future.
The Power of Together,
David S. Guzick, M.D., Ph.D. UF Senior Vice President for Health Affairs President, UF Health
About the author
