Definition
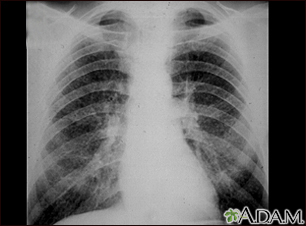
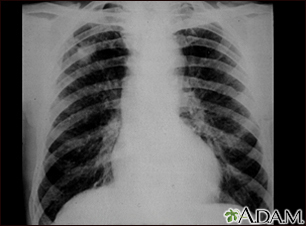
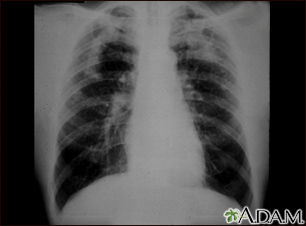
Interstitial lung disease (ILD) is a group of lung disorders in which the lung tissues become inflamed and then damaged.
Alternative Names
Diffuse parenchymal lung disease; Alveolitis; Idiopathic pulmonary pneumonitis (IPP)
Causes
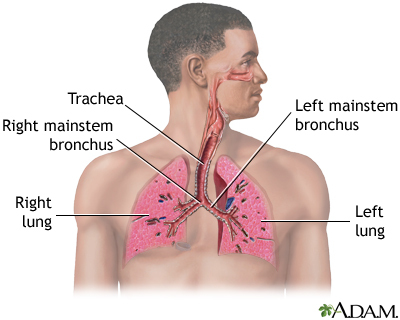
The lungs contain tiny air sacs (alveoli), which is where oxygen is absorbed. These air sacs expand with each breath.
The tissue around these air sacs is called the interstitium. In people with interstitial lung disease, this tissue becomes stiff or scarred, and the air sacs are not able to expand as much. As a result, not as much oxygen can get to the body.
ILD can occur without a known cause. This is called idiopathic ILD. Idiopathic pulmonary fibrosis (IPF) is the most common disease of this type.
There are also dozens of known causes of ILD, including:
- Autoimmune diseases (in which the immune system attacks the body) such as lupus, rheumatoid arthritis, sarcoidosis, and scleroderma.
- Lung inflammation due to breathing in a foreign substance such as certain types of dust, fungus, or mold (hypersensitivity pneumonitis).
- Medicines (such as nitrofurantoin, sulfonamides, bleomycin, amiodarone, methotrexate, gold, infliximab, etanercept, and other chemotherapy medicines).
- Radiation treatment to the chest.
- Working with or around asbestos, coal dust, cotton dust, and silica dust (called occupational lung disease).
- Infection and partial recovery from diseases like COVID-19.
Cigarette smoking may increase the risk of developing some forms of ILD and may cause the disease to be more severe.
Symptoms
Shortness of breath is a main symptom of ILD. You may breathe faster or need to take deep breaths:
- At first, shortness of breath may not be severe and is only noticed with exercise, climbing stairs, and other activities.
- Over time, it can occur with less strenuous activity such as bathing or dressing, and as the disease worsens, even with eating or talking.
Most people with this condition also have a dry cough. A dry cough means you do not cough up any mucus or sputum.
Over time, weight loss, fatigue, and muscle and joint pain are also present.
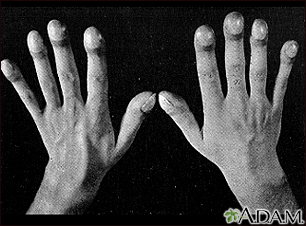
People with more advanced ILD may have:
- Abnormal enlargement and curving of the base of the fingernails (clubbing).
- Blue color of the lips, skin, or fingernails due to low blood oxygen levels (cyanosis).
- Symptoms of the other diseases such as arthritis or trouble swallowing (scleroderma), associated with ILD.
Exams and Tests
The health care provider will perform a physical exam. Dry, crackling breath sounds may be heard when listening to the chest with a stethoscope.
The following tests may be done:
People who are heavily exposed to known causes of lung disease in the workplace are usually routinely screened for lung disease. These jobs include coal mining, sand blasting, and working on a ship.
Treatment
Treatment depends on the cause and duration of the disease. Medicines that suppress the immune system and reduce swelling in the lungs are prescribed if an autoimmune disease is causing the problem. For some people who have IPF, pirfenidone and nintedanib are two medicines that may be used to slow the disease. If there is no specific treatment for the condition, the aim is to make you more comfortable and support lung function:
Lung rehabilitation can provide support, and help you learn:
- Different breathing methods
- How to set up your home to save energy
- How to eat enough calories and nutrients
- How to stay active and strong
Some people with advanced ILD may need a lung transplant.
Support Groups
You can ease the stress of illness by joining a support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
The chance of recovering or ILD getting worse depends on the cause and how severe the disease was when it was first diagnosed.
Some people with ILD develop heart failure and high blood pressure in the blood vessels of their lungs (pulmonary hypertension).
Idiopathic pulmonary fibrosis has a poor outlook.
References
Corte TJ, Wells AU. Connective tissue diseases. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 92.
Graney BA, Lee JS, King TE. Nonspecific interstitial pneumonitis and other idiopathic interstitial pneumonias. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 90.
Raghu G, Martinez FJ. Interstitial lung disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 86.