Treatment
Treatment options for complex aortic aneurysms vary and include medical management (monitoring the aneurysm while controlling blood pressure), open surgery and catheter-based endovascular repair.
Endovascular repair
Your health care provider has recommended an endovascular repair. This is a minimally invasive procedure and when performed to repair a complex aortic aneurysm, it is known as a FEVAR, or fenestrated endovascular aortic repair. Traditional endovascular repair involves inserting a stent graft into the aneurysm. Because your aneurysm involves the major vessels that arise from the aorta to feed the kidneys, intestines and liver, these stent grafts cannot be used because they would block blood flow to these organs. Instead, a fenestrated endograft will be used. These grafts have openings, or fenestrations, or graft branches that align with the arteries branching off of the aorta through which smaller stent grafts are connected to the aortic branches, allowing blood flow to continue.
Without the use of branched or fenestrated endovascular grafts, repair of aortic aneurysms in this area of the body requires extensive open surgery. Many patients are not candidates for an open aneurysm repair because of the magnitude of the operation, and these patients may have no other options for repair. Thus, this invasive procedure allows treatment for patients who previously were not aneurysm repair candidates.
Procedure
Before the procedure
Here are some tips and information that will help your procedure be as successful as possible:
- The evening before your surgery, you may eat a normal dinner. However, you cannot eat or drink anything, including water, gum or hard candy, beginning at midnight prior to your operation.
- Bring a list of your current medications that includes the names, dosages and
how often you take them.
- Talk to your physician about possible drug interactions. If you are taking anticoagulant (blood-thinning) medication such as Warfarin, Coumadin or antiplatelet medication such as Plavix or Aspirin, you may be asked to stop taking them because they make it more difficult for your blood to clot.
- Talk to your health care provider about which medications you should stop and for how long. You should also ask your health care provider which medications you should still take on the day of your surgery.
- You will be given a special soap to wash with the day before your surgery, which decreases bacteria on your skin and may help reduce the risk of infection after your procedure.
- For the comfort and safety of all patients, UF Health requests that you do not bring jewelry, valuables, electric appliances (hair dryer, shaver, heating pads, etc.), food or medications with you on the day of your procedure.
- Shortly before your scheduled time of surgery, you will be taken to the pre-op care unit. An intravenous, or IV, line may be started before the procedure to provide fluid and any pre-op medications you have not yet received.
- Before going to the operating room, remove all jewelry, including rings. You may wear your glasses/contacts, dentures and/or hearing aids until you go to surgery so you can communicate with members of the team in the preparation area. Prior to going to the operating room, your pre-op nurse will give these items to your family until you need them during recovery.
Procedure
General anesthesia is used so you will be asleep during the procedure. To prevent spinal cord ischemia (paralysis), by decreasing spinal cord pressure, a spinal drain may be placed in your back, if indicated.
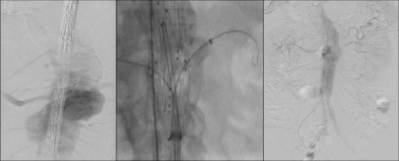
Incisions may be created in one or both of your groins and you may also have an incision on your arm or in your axilla (armpit). Using wires and catheters, the aorta will be accessed through these small incisions. X-rays will be taken using a special contrast dye that helps visualize blood vessels (Figure 3). Under this direct visualization, a stent graft is guided over the wires into the aorta, it is positioned and deployed. Next, wires are placed through the graft fenestrations or branches and smaller stent grafts that connect to the branch vessels are deployed. This allows exclusion of the aortic aneurysm while preserving blood flow to all the abdominal organs.
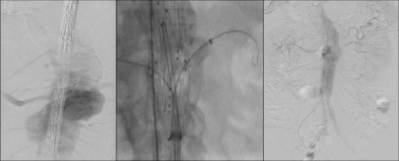
Figure 3. X-rays will be taken using a special contrast
dye that helps visualize blood vessels.
After the procedure
You will be taken to the intensive care unit, or ICU. Once you are ready to leave the ICU, typically in a day or two, you will be moved to a medical-surgical unit to complete your recovery. You are asked to lay flat in bed until the spinal drain has been discontinued, usually 24-48 hours after your procedure. When you are tolerating a diet and able to walk, you will be able to leave the hospital. A typical stay will last from three to seven days, depending on the complexity of the repair.
There are risks associated with every procedure. Those specific to this operation include, but are not limited to:
- Weakness or complete paralysis of legs
- Transient issues with the kidneys secondary to the dye (contrast)
- Problems with the arteries to the intestine
- Endoleak (poor seal/apposition of the graft to the arterial wall)
- Infection of the groin incision
- Bleeding
Post-Operative Care
For two weeks after the endovascular repair, you should not lift anything that more than five to 10 pounds. If you are taking narcotic medications, do not or operate heavy machinery as these medications can impair judgment. You may shower and let soap and water run over your incisions, but must pat them dry. You may return to work when you are cleared by your doctor. Check your incision daily for signs of infection (redness, increased tenderness, warmth or swelling). If you develop sudden shortness of breath or chest pain, or if notice changes in color, sensation or strength in your legs, please seek medical attention immediately.
Follow-up
Over time, stent grafts may have problems such as kinking, migration or leakage and you may or may not experience symptoms. Therefore, you will need lifelong routine surveillance.
At the time of discharge, you will be provided an appointment at one month and six months from the date of repair with a repeat CT scan to evaluate the stent graft and remodeling of the aorta around the graft. After that, follow-up will be done yearly. It is crucial that you are compliant with the follow-up plan provided to you to ensure the most successful outcome after your procedure.
If you develop an endoleak, the aneurysm may continue to grow after the, and may result in rupture. This is why it is so important to be compliant with your routine follow-up as directed by your physician. Most endoleaks can be treated by a simple, minimally invasive treatment.
Download a PDF of our FEVAR patient guide (PDF).