Bone mineral density test
Definition
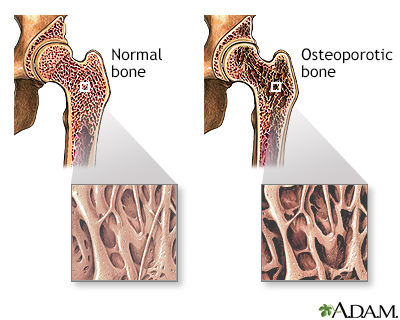
A bone mineral density (BMD) test measures how much calcium and other types of minerals are in an area of your bone.
This test helps your health care provider detect osteoporosis and predict your risk for bone fractures.
Patient Education Video: Osteoporosis
Alternative Names
BMD test; Bone density test; Bone densitometry; DEXA scan; DXA; Dual-energy x-ray absorptiometry; p-DEXA; Osteoporosis - BMD; Dual x-ray absorptiometry
How the Test is Performed
Bone density testing can be done in several ways.
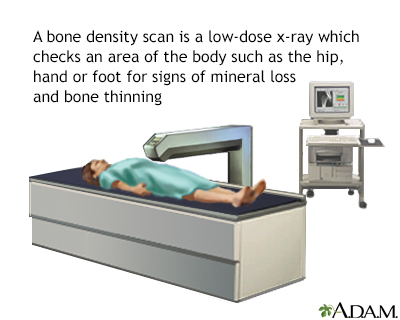
The most common and accurate way uses a dual-energy x-ray absorptiometry (DEXA) scan. DEXA uses low-dose x-rays. (You receive more radiation from a chest x-ray.)
There are two types of DEXA scans:
- Central DEXA -- You lie on a soft table. The scanner passes over your lower spine and hip. In most cases, you do not need to undress. This scan is the best test to predict your risk for fractures, especially of the hip.
- Peripheral DEXA (p-DEXA) -- These smaller machines measure the bone density in your wrist, fingers, leg, or heel. These machines are in health care offices, pharmacies, shopping centers, and at health fairs.
How to Prepare for the Test
If you are or could be pregnant, tell your provider before this test is done.
DO NOT take calcium supplements for 24 hours before the test.
You'll be told to remove all metal items from your body, such as jewelry and buckles.
How the Test will Feel
The scan is painless. You need to remain still during the test.
Why the Test is Performed
Bone mineral density (BMD) tests are used to:
- Diagnose bone loss and osteoporosis
- See how well osteoporosis medicine is working
- Predict your risk for future bone fractures
Bone density testing is recommended for all women age 65 and older.
There is not full agreement on whether men should undergo this type of testing. Some groups recommend testing of men at age 70, while others state that the evidence is not clear enough to say whether men at this age benefit from screening.
Younger women, as well as men of any age, may also need bone density testing if they have risk factors for osteoporosis. These risk factors include:
- Fracturing a bone after age 50
- Strong family history of osteoporosis
- History of treatment for prostate cancer or breast cancer
- History of medical conditions such as rheumatoid arthritis, diabetes, thyroid imbalances, or anorexia nervosa
- Early menopause (either from natural causes or hysterectomy)
- Long-term use of medicines such as corticosteroids, thyroid hormone, or aromatase inhibitors
- Low body weight (less than 127 pounds or 57 kilograms) or low body mass index (less than 21)
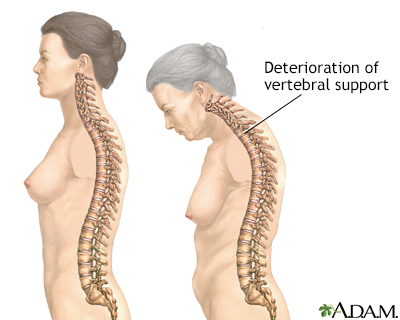
- Significant loss of height
- Long-term tobacco or excessive alcohol use
Normal Results
The results of your test are usually reported as a T-score and Z-score:
- T-score compares your bone density with that of a healthy young woman.
- Z-score compares your bone density with that of other people of your age, sex, and race.
With either score, a negative number means you have thinner bones than average. The more negative the number, the higher your risk for a bone fracture.
A T-score is within the normal range if it is -1.0 or above.
What Abnormal Results Mean
Bone mineral density testing does not diagnose fractures. Along with other risk factors you may have, it helps predict your risk for having a bone fracture in the future. Your provider will help you understand the results.
If your T-score is:
- Between -1 and -2.5, you may have early bone loss (osteopenia)
- Below -2.5, you likely have osteoporosis
Treatment recommendation depends on your total fracture risk. This risk can be calculated using the FRAX score. Your provider can tell you more about this. You can also find information about FRAX online.
Risks
Bone mineral density uses a slight amount of radiation. Most experts feel that the risk is very low compared with the benefits of finding osteoporosis before you break a bone.
Gallery
References
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364-376. PMID: 30696576 pubmed.ncbi.nlm.nih.gov/30696576/.
Kendler D, Almohaya M, Almehthel M. Dual x-ray absorptiometry and measurement of bone. In: Hochberg MC, Gravallese EM, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH, eds. Rheumatology. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 51.
US Preventive Services Task Force; Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(24):2521-2531. PMID: 29946735 pubmed.ncbi.nlm.nih.gov/29946735/.
Weber TJ. Osteoporosis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 230.