Exploring the Sinus Microbiome in Chronic Sinusitis
Researchers at the University of Florida are among the first investigators to examine the clinical and microbiologic characteristics, risk factors and…

Update your location to show providers, locations, and services closest to you.
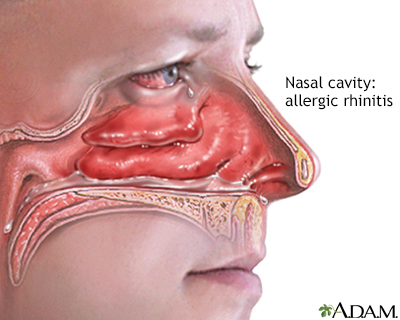
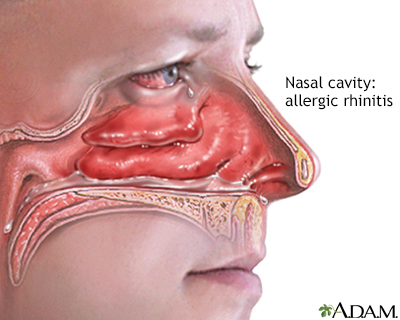
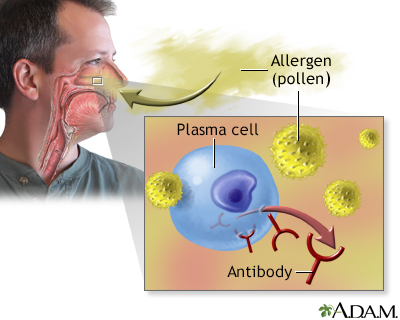
Allergic rhinitis is a diagnosis associated with a group of symptoms affecting the nose. These symptoms occur when you breathe in something you are allergic to, such as dust, animal dander, or pollen. Symptoms can also occur when you eat a food that you are allergic to.
This article focuses on allergic rhinitis due to plant pollens. This type of allergic rhinitis is commonly called hay fever or seasonal allergy.
Hay fever; Nasal allergies; Seasonal allergy; Seasonal allergic rhinitis; Allergies - allergic rhinitis; Allergy - allergic rhinitis
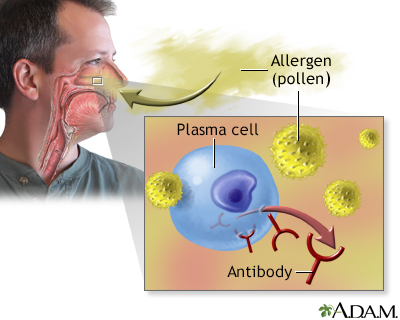
An allergen is something that triggers an allergy. When a person with allergic rhinitis breathes in an allergen such as pollen, mold, animal dander, or dust, the body releases chemicals that cause allergy symptoms.
Hay fever involves an allergic reaction to pollen.
Plants that cause hay fever are trees, grasses, and ragweed. Their pollen is carried by the wind. (Flower pollen is carried by insects and does not cause hay fever.) Types of plants that cause hay fever vary from person to person and from area to area.
The amount of pollen in the air can affect whether hay fever symptoms develop or not.
Hay fever and allergies often run in families. If both of your parents have hay fever or other allergies, you are likely to have hay fever and allergies, too. The chance is higher if your mother has allergies.
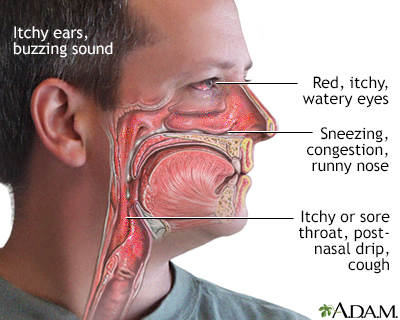
Symptoms that occur shortly after you come into contact with the substance you are allergic to may include:
Symptoms that may develop later include:
The health care provider will perform a physical exam and ask about your symptoms. You will be asked whether your symptoms vary by time of day or season, and exposure to pets or other allergens.
Allergy testing may reveal the pollen or other substances that trigger your symptoms. Skin testing is the most common method of allergy testing.
If your doctor determines you cannot have skin testing, special blood tests may help with the diagnosis. These tests, known as IgE RAST tests, can measure the levels of allergy-related substances.
A complete blood count (CBC) test, called the eosinophil count, may also help diagnose allergies.
LIFESTYLE AND AVOIDING ALLERGENS
The best treatment is to avoid the pollens that cause your symptoms. It may be impossible to avoid all pollen. But you can often take steps to reduce your exposure.
You may be prescribed medicine to treat allergic rhinitis. The medicine your doctor prescribes depends on your symptoms and how severe they are. Your age and whether you have other medical conditions, such as asthma, will also be considered.
For mild allergic rhinitis, a nasal wash can help remove mucus from the nose. You can buy a saline solution at a drug store or make one at home using 1 cup (240 milliliters) of warm water, half a teaspoon (3 grams) of salt, and pinch of baking soda.
Treatments for allergic rhinitis include:
ANTIHISTAMINES
Medicines called antihistamines work well for treating allergy symptoms. They may be used when symptoms do not happen often or do not last long. Be aware of the following:
CORTICOSTEROIDS
DECONGESTANTS
OTHER MEDICINES
ALLERGY SHOTS
Allergy shots (immunotherapy) are sometimes recommended if you cannot avoid the pollen and your symptoms are hard to control. This includes regular shots of the pollen you are allergic to. Each dose is slightly larger than the dose before it, until you reach the dose that helps control your symptoms. Allergy shots may help your body adjust to the pollen that is causing the reaction.
SUBLINGUAL IMMUNOTHERAPY TREATMENT (SLIT)
Instead of shots, medicine put under the tongue may help for grass and ragweed allergies.
Most symptoms of allergic rhinitis can be treated. More severe cases need allergy shots.
Some people, especially children, may outgrow an allergy as the immune system becomes less sensitive to the trigger. But once a substance such as pollen causes allergies, it often continues to have a long-term effect on the person.
Contact your provider for an appointment if:
You can sometimes prevent symptoms by avoiding the pollen you are allergic to. During pollen season, you should stay indoors where it is air-conditioned, if possible. Sleep with the windows closed, and drive with the windows rolled up.
Cox DR, Wise SK, Baroody FM. Allergy and immunology of the upper airway. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head & Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 35.
Milgrom H, Sicherer SH. Allergic rhinitis. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 168.
Wallace DV, Dykewicz MS, Oppenheimer J, Portnoy JM, Lang DM. Pharmacologic treatment of seasonal allergic rhinitis: synopsis of guidance from the 2017 joint task force on practice parameters. Ann Intern Med. 2017;167(12):876-881. PMID: 29181536 pubmed.ncbi.nlm.nih.gov/29181536/.



Researchers at the University of Florida are among the first investigators to examine the clinical and microbiologic characteristics, risk factors and…

Spring has sprung! For most people that means beautiful weather, outdoor activities and blooming flowers. For about 50 million adults that means sneezing,…